eISSN: 2093-8462 http://jesk.or.kr
Open Access, Peer-reviewed
eISSN: 2093-8462 http://jesk.or.kr
Open Access, Peer-reviewed
Woo Jin Kim
, Byung Yong Jeong
, Jiyoung Park
10.5143/JESK.2023.42.6.587 Epub 2024 January 06
Abstract
Objective: The purpose of this study is to conduct a systematic literature review in order to understand the communication characteristics of nurses, including measurement tools, subjects, influencing factors, and improvement strategies.
Background: Nurses assist doctors in medical treatments, adhering to prescribed medical interventions and established nursing procedures. They also take emergency measures in the absence of physicians, monitor and document patients' conditions, and provide explanations about treatments and disease prevention to patients and their families. The role of a nurse encompasses these responsibilities, underscoring the significance of effective communication skills during the execution of these tasks.
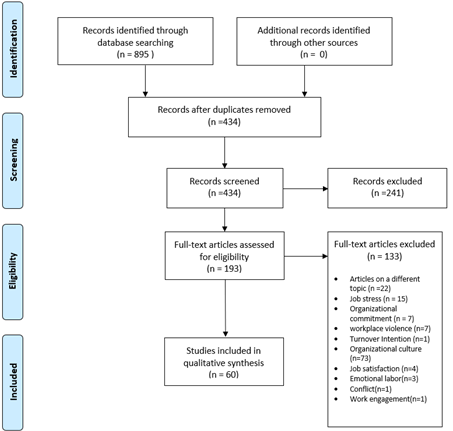
Method: The study was conducted based on research articles retrieved from academic paper databases such as KISS, DBPIA, RISS, and KCI, using the search query on September 2, 2022. The search query used for selecting the articles was as follows: ((nurse AND hierarchy) OR (nurse AND patient AND communication) OR (nurse AND physician AND communication)). A total of 895 research articles were retrieved from academic paper databases on September 2, 2022, with 135 from KISS, 370 from DBPIA, 301 from RISS, and 89 from KCI. After removing duplicate articles, 434 articles remained for consideration. Among these, 374 articles were excluded based on inclusion and exclusion criteria, resulting in a final selection of 60 articles. These 60 articles were utilized for conducting a systematic literature review.
Results: In this study, we examined communication assessment tools, communication proficiency, factors influencing communication, and potential improvement strategies. The GICC was the most frequently used communication assessment tool. Communication proficiency was found to be highest in the miscellaneous ward, while informal communication methods were less common. Factors influencing communication were identified as personal and organizational characteristics. Proposed strategies for improving communication included educational programs for enhancing communication skills, expressing opinions to supervisors, and activating informal organizational networks.
Conclusion: This study conducted a comprehensive literature review to examine the communication level of nurses, their communication subjects, influencing factors on communication, and potential avenues for improvement. Through this research, it is anticipated that the study's findings can serve as foundational data for enhancing deteriorated working environments due to communication issues among nurses.
Application: The aim of this study is to provide foundational data for addressing the physical consequences (such as assault, punctures, cuts) and psychological health issues (emotional exhaustion, verbal abuse) experienced by nurses due to inappropriate communication. The goal is to offer solutions that enable them to work in a safer and healthier working environment.
Keywords
간호사는 의사의 진료를 지원하며 의사의 처방에 따라 환자 치료를 수행하고, 의사가 부재할 경우 비상 조치를 취하기도 한다. 또한, 환자 상태를 지속적으로 모니터링하고 기록하며, 환자와 그 가족에게 치료 및 질병 예방에 대한 설명을 제공한다. 이러한 업무를 수행함에 있어서 의사소통 능력은 매우 중요하다(Statistics Korea, 2017). 더불어, 간호사는 환자와 함께 동료 간호사 뿐만 아니라 의사, 약사, 간호조무사, 영양사, 사회복지사 및 행정부서 직원과 협력하여 업무를 수행하므로 효과적인 의사소통 능력은 필수적이다(Lee et al., 2013; Brown et al., 2009).
간호사의 의사소통 문제는 직무 만족도를 저하시키며 직무 스트레스, 업무적 소진, 직장 내 폭력 등의 원인이 되어 작업자의 건강과 안전에 부정적인 영향을 미칠 수 있다(Samur and Intepeler, 2017). 또한, 간호사는 동료나 환자와의 의사소통 문제로 인해 정신질환과 심리적 건강 장애가 발생할 수도 있다(An et al., 2020).
간호사의 의사소통 특성에 관한 연구들은 주로 간호서비스 품질 및 업무 성과 향상을 목표로 하며, 이를 체계적으로 종합하여 정리한 연구는 아직 부족한 상태입니다. 본 연구에서는 국내 병원에 종사하는 간호사의 의사소통 특성을 알아보기 위하여 국내 학술논문데이터베이스를 활용한 체계적인 문헌고찰을 실시하고자 한다. 이를 통해, 간호사의 의사소통을 측정하는 도구와 의사소통 대상, 영향 요인, 개선방안 등의 특성을 파악하고자 한다.
2.1 Research strategy
KISS, DBPIA, RISS, KCI의 학술논문데이터베이스에서 아래의 검색식으로 2022년 9월 2일에 검색한 논문을 대상으로 연구를 진행하였다((간호사 AND 조직문화) OR(간호사 AND 위계서열) OR(간호사 AND 환자 AND 의사소통) OR(간호사 AND 의사 AND 의사소통)).
2.2 Research question
국내 간호사의 의사소통 특성을 알아보기 위해 활용된 의사소통 측정도구, 의사소통 대상, 의사소통 영향요인 및 개선방안을 파악하고자 한다.
2.3 Selected articles
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses)에 따른(Moher et al., 2009) 체계적 문헌고찰을 위한 논문 선택의 흐름도는 Figure 1과 같다. 연구를 진행하기 위해 2022년 9월 2일에 학술논문데이터베이스에서 검색된 논문은 KISS 135개, DBPIA 370개, RISS 301개, KCI 89개, 총 895개이며, 선택된 논문의 참고문헌 중에서 포함되어야 하는 기준에 적합한 추가 논문은 없었다. 중복된 논문을 제외한 434개의 논문이 선택되었다. 434개의 논문의 초록을 확인하여 포함기준과 제외기준에 따라 총 374개가 제외하였으며, 최종 60개의 논문을 채택하였다. 최종적으로 채택된 60개 논문은 원문을 확인하여 체계적인 문헌고찰을 진행하였다.
3.1 Communication measuring tool
최종 선택된 논문에 사용된 의사소통 측정도구는 Table 1과 같이 정리하였다. 총 60편 논문 중 글로벌 인간관계 의사소통능력 측정도구(Global Interpersonal Communication Competence, GICC)를 이용하여 연구한 논문이 32편으로 가장 많았고, 간호사의 조직 내 의사소통 측정도구 5편, 의사소통 유형 측정도구 4편, 간호사의 의사소통갈등 측정도구 3편, ICU Nurse-Physician Questionnaire의 의사소통 도구, Primary Communication Inventory (PCI), 구체적 의사소통행위 도구, 촉진적 의사소통 검사지가 각 2편, 그 외 간호사의 의사소통 유형 측정도구, 상담자 자기평가 질문지(Counseling Self-Estimate Inventory, COSE), 언어적 및 비언어적 의사소통 측정도구, 의사소통 분류 유형(상향적, 하향적, 수평적, 비공식적)에 따른 측정도구, 의사소통 훈련 요구 측정도구, 생애능력 측정도구(주도적 의사소통), 의사소통 척도 측정도구, 의사소통능력진단 도구, 의사소통장애요인 측정도구, 치매대상자를 돌보는 간호사의 행위 측정도구를 활용한 논문이 각 1편씩으로 조사되었다.
Measuring
tool |
Author (Year) |
Question |
Scale |
|
GICC |
Han and Kim (2022); Kim and Park (2022); Kim |
15 |
Likert 5 Scale |
|
Im and Kim (2008) |
48 |
Likert 5 Scale |
|
|
ICU Nurse-Physician Questionnaire's |
Yoo (2022) |
19 |
Likert 5 Scale |
|
Cho et al. (2013) |
30 |
Likert 5 Scale |
|
|
Primary Communication Inventory |
Lee and Lee (2016); Jung and Shin (2011) |
25 |
Likert 5 Scale |
|
Tools to measure nurses' communication patterns |
Park and Lee (2011) |
18 |
Likert 5 Scale |
|
Nurse's Communication Conflict Measurement Tool |
Oh and Choi (2018); Koo and Kim (2014); |
36 |
Likert 5 Scale |
|
Tools to measure nurses' intra-organizational
communication |
Lee and Ji (2021); Park and Lee (2018); |
24 |
Likert 5 Scale |
|
Go et al. (2022) |
20 |
Likert 5 Scale |
|
|
Specific communication tools |
Oh and Choi (2018) |
18 |
Likert 5 Scale |
|
Oh et al. (2016) |
20 |
Likert 5 Scale |
|
|
A communication skills measurement |
Ahn (2017) |
13 |
Likert 5 Scale |
|
Communication Type |
Lee and Kim (2010); Jeong and Kim (2009); |
35 |
Likert 5 Scale |
|
Kim et al. (2004) |
12 |
Likert 5 Scale |
|
|
Communication Training Needs |
Hyeon (2002) |
10 |
Likert 5 Scale |
|
Life Skills Assessment Tool: |
Yune et al. (2018) |
7 |
Likert 5 Scale |
|
Communication Skills Scale |
Kim et al. (2016) |
49 |
Likert 5 Scale |
|
Communication Skills Diagnostic Tool |
Ha and Jeon (2016) |
35 |
Likert 5 Scale |
|
Tools for communication disorder factors |
Kim et al. (2017) |
58 |
Likert 5 Scale |
|
Facilitated Communication Test |
Jeong et al (2012); Park and Yang
(2008) |
49 |
Likert 5 Scale |
|
Communication behavior scale of |
Lee and Gang (2018) |
18 |
Likert 5 Scale |
|
Note GICC:
Global Interpersonal Communication Competence |
|||
3.2 Communication target and level of communication
간호사의 의사소통 대상 및 수준이 업무와 환경 등에서 차이가 나타나는 점을 고려하여 근무부서 별로 의사소통 대상, 의사소통 도구, 의사소통 수준을 정리하였다. 공식적 의사소통은 상향식, 하향식, 수평적 의사소통을 말하며, 비공식적 의사소통으로 분류한다(Lee and Kim, 2010; Kim, 2005; Mathis and Jackson, 2010). 개방성은 간호사와 의사가 서로 이야기할 때 어떤 두려움이나 오해 없이 진실을 표현할 수 있는 정도를 나타낸다(Shortell et al., 1991; Roberts and O'Reilly, 1974). 또한, 정확성은 간호사와 의사가 상대방에 의해 전달된 정보의 정확성을 신뢰하는 정도를 의미한다(Shortell et al., 1991; Roberts and O'Reilly, 1974).
3.2.1 Medical ward
Table 2는 내과병동의 의사소통 대상과 수준을 정리한 것이다. Table 2와 같이 내과병동에서 사용빈도가 높은 의사소통 측정도구는 글로벌 인간관계 의사소통능력 측정도구(GICC)가 6편으로 가장 높게 나타났고, 간호사의 조직 내 의사소통 측정도구 2편, 의사소통 유형 측정도구 2편, ICU Nurse-Physician Questionnaire의 의사소통 도구 2편 순으로 나타났다. 의사소통 대상은 간호사가 11편으로 가장 높게 나타났고, 환자 6편, 의사 5편, 보호자 3편, 보건의료종사자와 의료직원에 관한 연구가 각각 1편으로 나타났다.
내과병동 간호사의 의사소통 수준은 3.23~3.85점으로 나타났다. 또한, 비공식(2.52~2.68점)적인 의사소통 보다 공식(3.00~3.55점)적인 의사소통 점수가 높게 나타났다. 개방성은 의사(2.68점)와의 의사소통보다 간호사(3.70점)와의 의사소통 점수가 높게 나타났다. 정확성도 의사(2.69)와의 의사소통보다 간호사(3.18점)와의 의사소통 점수가 높게 나타났다. 간호사 조직 내의 의사소통 점수는 3.27~3.29점으로 나타났다.
|
Communication |
Measuring tool |
Level of communication (Mean ± SD) |
Author (Year) |
|
Patient, Guardian, |
GICC |
3.27±0.40 |
Lee et al. (2013) |
|
Doctor, Nurse, |
GICC |
3.48±0.33 |
Lee and Kim (2010) |
|
- |
GICC |
3.71±0.67 |
Han (2019) |
|
Patient, Nurse |
GICC |
3.38±0.46 |
Kim and Lee (2014) |
|
Patient, Nurse |
GICC |
3.23±0.33 |
Park and Chung |
|
Patient, Nurse, |
GICC |
3.27±0.62 |
Shin (2018) |
|
Nurse, medical staff |
Tools to measure nurses' |
3.27±0.48 |
Lee and Ji (2021) |
|
Nurse, Doctor |
Tools to measure nurses' |
3.29±0.40 |
Yoon et al. (2018) |
|
Doctor, Nurse, |
Communication Type Measurement Tool |
Formal 3.25±0.40 |
Lee and Kim (2010) |
|
Nurse |
Communication Type Measurement Tool |
Upward 3.06±0.62 |
Seo et al. (2003) |
|
Nurse, Doctor |
ICU Nurse-Physician Questionnaire's
Communication |
Openness (Nurse-Physician) 2.68±0.77 |
Cho et al. (2013) |
|
Doctor, Nurse |
ICU Nurse-Physician Questionnaire's
Communication |
Openness 2.98±0.69 Accuracy 2.75±0.54 Mutual understanding Timeliness 3.81±0.52 |
Yoo (2022) |
|
Note GICC: Global Interpersonal Communication
Competence |
|||
3.2.2 Surgical ward
Table 3은 외과병동의 의사소통 대상과 수준을 정리한 것이다. Table 3과 같이 외과병동에서 사용빈도가 높은 의사소통 측정도구는 글로벌 인간관계 의사소통능력 측정도구(GICC)가 6편으로 가장 높게 나타났고, 간호사의 조직 내 의사소통 측정도구 2편, 의사소통 유형 측정도구 2편, ICU Nurse-Physician Questionnaire의 의사소통 도구 2편 순으로 나타났다. 의사소통 대상은 간호사가 11편으로 가장 높게 나타났고, 환자 6편, 의사 5편, 보호자 3편, 보건의료종사자와 의료직원이 각각 1편 순으로 나타났다. 외과병동 간호사의 의사소통 수준은 3.14~3.82점으로 나타났다. 또한, 비공식적인(2.68~2.73점) 의사소통 점수보다 공식적인(3.00~3.55점) 의사소통 점수가 높게 나타났다. 개방성은 의사(2.75점)와의 의사소통보다 간호사(3.75점)와의 의사소통 점수가 높게 나타났다. 정확성도 의사(2.63점)와의 의사소통보다 간호사(3.20점)와의 의사소통 점수가 높게 나타났다. 간호사 조직 내의 의사소통 점수는 3.14~3.32점으로 나타났다.
|
Communication |
Measuring tool |
level of communication (Mean ± SD) |
Author (Year) |
|
Doctor, Nurse, |
GICC |
3.51±0.37 |
Lee and Kim (2010) |
|
Patient, Guardian, |
GICC |
3.32±0.44 |
Lee et al. (2013) |
|
- |
GICC |
3.58±0.45 |
Han (2019) |
|
Patient, Nurse |
GICC |
3.41±0.44 |
Kim and Lee (2014) |
|
Patient, Nurse |
GICC |
3.23±0.31 |
Park and Chung |
|
Patient, Nurse, |
GICC |
3.26±0.61 |
Shin (2018) |
|
Nurse, medical staff |
Tools to measure nurses' |
3.14±0.49 |
Lee and Ji (2021) |
|
Nurse, Doctor |
Tools to measure nurses' intra-organizational communication |
3.32±0.45 |
Yoon et al. (2018) |
|
Doctor, Nurse, |
Communication Type |
Formal 3.27±0.39 |
Lee and Kim (2010) |
|
Nurse |
Communication Type |
Upward 3.06±0.62 |
Seo et al. (2003) |
|
Doctor, Nurse |
ICU Nurse-Physician Questionnaire's Communication |
Openness 2.57±0.61 Accuracy 2.75±0.62 Mutual
understanding Timeliness 3.74±0.55 |
Yoo (2022) |
|
Nurse, Doctor |
ICU Nurse-Physician Questionnaire's Communication |
Openness (Nurse-Physician) 2.75±0.74 |
Cho et
al. (2013) |
|
Note GICC: Global Interpersonal
Communication Competence |
|||
3.2.3 Medical and surgical ward
Table 4는 내외과병동의 의사소통 대상과 수준을 정리한 것이다. Table 4와 같이 내외과병동에서 사용빈도가 높은 의사소통 측정도구는 글로벌 인간관계 의사소통능력 측정도구(GICC)가 4편으로 가장 높게 나타났고, 간호사의 의사소통갈등 측정도구 1편, 간호사의 조직 내 의사소통 측정도구 1편 순으로 나타났다. 의사소통 대상은 간호사가 3편으로 가장 높게 나타났고, 의사와 의료직원이 각각 1편 순으로 나타났다. 내외과병동 간호사의 의사소통 수준은 3.27~3.79점으로 나타났다. 또한, 간호사 간의 의사소통갈등 점수가 3.50점으로 나타났다. 간호사 조직 내의 의사소통 점수는 3.27점으로 나타났다.
|
Communication target |
Measuring tool |
Level of communication |
Author
(Year) |
|
Medical staff |
GICC |
3.53±0.32 |
Lim and Yi (2014) |
|
- |
GICC |
3.79±0.59 |
Han (2019) |
|
- |
GICC |
3.47±0.40 |
Kim et al. (2018b) |
|
Nurse, Doctor |
GICC |
3.43±0.41 |
Lee and Kim (2017) |
|
Nurse |
Nurse's Communication Conflict Measurement Tool |
3.50±0.53* |
Koo and Kim (2014) |
|
Nurse |
Tools to measure nurses' intra- |
3.27±0.46 |
Go et al. (2022) |
|
Note *: reverse question, GICC: Global
Interpersonal Communication Competence |
|||
3.2.4 Other ward
Table 5는 기타병동(호스피스병동, 노인병동, 정신병동 등)의 의사소통 대상과 수준을 정리한 것이다. Table 5와 같이 기타병동에서 사용빈도가 높은 의사소통 측정도구는 글로벌 인간관계 의사소통능력 측정도구(GICC)가 5편으로 가장 높게 나타났고, 간호사의 의사소통갈등 측정도구 1편 순으로 나타났다. 의사소통 대상은 간호사와 환자가 각각 4편으로 가장 높게 나타났고, 암환자와 보호자, 보건의료종사자가 각각 1편 순으로 나타났다. 기타병동 간호사의 의사소통 수준은 3.47~3.79점으로 나타났다. 또한, 간호사 간의 의사소통갈등 점수가 3.32점으로 나타났다.
|
Communication target |
Measuring tool |
Level of communication |
Author (Year) |
|
Cancer patient |
GICC |
3.68±0.43 |
Kang and Jung (2019) |
|
- |
GICC |
3.56±0.47 |
Jung (2019) |
|
Patient, Guardian, Nurse |
GICC |
3.47±0.49 |
Nam et al. (2020) |
|
Patient, Nurse |
GICC |
3.65±0.36 |
Kang and Kim (2016) |
|
Patient, Nurse |
GICC |
3.79±0.40 |
Park (2018) |
|
Nurse, Patient, |
Nurse's Communication Conflict Measurement Tool |
3.32±0.49* |
Oh and Choi (2018) |
|
Note *: reverse question, GICC: Global
Interpersonal Communication Competence |
|||
3.2.5 Emergency room
Table 6은 응급실의 의사소통 대상과 수준을 정리한 것이다. Table 6과 같이 응급실에서 사용빈도가 높은 의사소통 측정도구는 ICU Nurse-Physician Questionnaire의 의사소통 도구가 2편으로 가장 높게 나타났고, 글로벌 인간관계 의사소통능력 측정도구(GICC) 1편, 간호사의 의사소통갈등 측정도구 1편, 의사소통 유형 측정도구 1편, 간호사의 조직 내 의사소통 측정도구 1편 순으로 나타났다. 의사소통 대상은 간호사가 6편으로 가장 높게 나타났고, 의사 3편, 환자 1편 순으로 나타났다. 응급실 간호사의 의사소통 수준은 3.10점으로 나타났다. 또한, 비공식적인(2.62점) 의사소통보다 공식적인(2.97~3.54점) 의사소통 점수가 높게 나타났다. 개방성은 의사(2.71점)와의 의사소통보다 간호사(3.66점)와의 의사소통 점수가 높게 나타났다. 정확성도 의사(2.77점)와의 의사소통보다 간호사(3.19점)와의 의사소통 점수가 높게 나타났다. 간호사 간의 의사소통갈등 점수가 3.50점으로 나타났다. 간호사 조직 내의 의사소통 점수는 3.21점으로 나타났다.
|
Communication target |
Measuring tool |
Level of communication (Mean ± SD) |
Author (Year) |
|
Nurse, Doctor |
ICU Nurse-Physician Questionnaire's Communication |
Openness (Nurse-Physician) 2.71±0.63 |
Cho et al. (2013) |
|
Doctor, Nurse |
ICU Nurse-Physician Questionnaire's Communication |
Openness 3.54±0.37 Accuracy 3.16±0.72 Mutual
understanding Timeliness 3.86±0.66 |
Yoo (2022) |
|
Patient, Nurse |
GICC |
3.10±0.22 |
Park and Chung |
|
Nurse |
Nurse's Communication Conflict Measurement Tool |
3.50±0.53* |
Koo and Kim (2014) |
|
Nurse |
Communication Type Measurement Tool |
Upward 3.03±0.62 |
Seo et al. (2003) |
|
Nurse, Doctor |
Tools to measure nurses' |
3.21±0.56 |
Yoon et al. (2018) |
|
Note *: reverse question, GICC: Global
Interpersonal Communication Competence |
|||
3.2.6 Outpatient
Table 7은 외래의 의사소통 대상과 수준을 정리한 것이다. Table 7과 같이 외래에서 사용빈도가 높은 의사소통 측정도구는 글로벌 인간관계 의사소통능력 측정도구(GICC)가 5편으로 가장 높게 나타났고, 간호사의 조직 내 의사소통 측정도구 1편, 의사소통 유형 측정도구 1편, ICU Nurse-Physician Questionnaire의 의사소통 도구 1편 순으로 나타났다. 의사소통 대상은 간호사가 6편으로 가장 높게 나타났고, 의사와 환자가 각각 2편, 보호자 1편 순으로 나타났다. 외래부서 간호사의 의사소통 수준은 3.28~3.66점으로 나타났다. 또한, 비공식적인(2.59점) 의사소통보다 공식적인(2.97~3.57점) 의사소통 점수가 높게 나타났다. 간호사 조직 내의 의사소통 점수는 2.96점으로 나타났다.
|
Communication target |
Measuring tool |
Level of communication (Mean ± SD) |
Author (Year) |
|
- |
GICC |
3.66±0.39 |
Han (2019) |
|
Patient, Nurse |
GICC |
3.48±0.35 |
Kim and Lee (2014) |
|
- |
GICC |
3.59±0.49 |
Kim
et al. (2018b) |
|
Nurse, Doctor |
GICC |
3.37±0.45 |
Lee and Kim (2017) |
|
Patient, Guardian, Nurse |
GICC |
3.28±0.48 |
Lee et al. (2013) |
|
Nurse |
Tools to measure nurses' |
2.96±0.67 |
Go et al. (2022) |
|
Nurse |
Communication Type |
Upward 3.27±0.37 |
Seo et al. (2003) |
|
Doctor, Nurse |
ICU Nurse-Physician Questionnaire's Communication |
Openness 3.14±0.63 Accuracy 2.93±0.67 Mutual understanding Timeliness 4.00±0.53 |
Yoo (2022) |
|
Note GICC: Global Interpersonal Communication Competence |
|||
3.2.7 Operation room
Table 8은 수술실의 의사소통 대상과 수준을 정리한 것이다.
|
Communication target |
Measuring tool |
Level of communication (Mean ± SD) |
Author (Year) |
|
Nurse, Doctor |
GICC |
3.46±0.41 |
Jung et al. (2020) |
|
Nurse |
GICC |
3.58±0.39 |
Kim and Cho (2021) |
|
Nurse, Doctor |
GICC |
3.37±0.45 |
Lee and Kim (2017) |
|
Medical staff |
GICC |
3.37±0.41 |
Lim and Yi (2014) |
|
- |
GICC |
3.78±0.34 |
Han (2019) |
|
Nurse, Doctor |
ICU Nurse-Physician |
Openness (Nurse-Physician) 3.28±0.58 |
Cho
et al. (2013) |
|
Doctor, Nurse |
ICU Nurse-Physician |
Openness 3.13±0.61 Accuracy 3.16±0.72 Mutual understanding Timeliness 3.61±0.59 |
Yoo (2022) |
|
Nurse, Doctor |
Tools to measure nurses' |
3.18±0.48 |
Yoon et al. (2018) |
|
Note GICC:
Global Interpersonal Communication Competence |
|||
Table 8과 같이 수술실에서 사용빈도가 높은 의사소통 측정도구는 글로벌 인간관계 의사소통능력 측정도구(GICC)가 5편으로 가장 높게 나타났고, 간호사의 조직 내 의사소통 측정도구 1편, ICU Nurse-Physician Questionnaire의 의사소통 도구 1편 순으로 나타났다. 의사소통 대상은 간호사가 6편으로 가장 높게 나타났고, 의사 5편, 의료직원 1편 순으로 나타났다. 수술실 간호사의 의사소통 수준은 3.37~3.78점으로 나타났다. 개방성은 의사(3.28점)와의 의사소통보다 간호사(3.59점)와의 의사소통 점수가 높게 나타났다. 정확성도 의사(2.69점)와의 의사소통보다 간호사(3.14점)와의 의사소통 점수가 높게 나타났다. 간호사 조직 내의 의사소통 점수는 3.18점으로 나타났다.
3.2.8 Intensive care unit
Table 9는 중환자실의 의사소통 대상과 수준을 정리한 것이다.
|
Communication target |
Measuring tool |
Level of communication (Mean ± SD) |
Author (Year) |
|
Patient, Nurse |
GICC |
3.16±0.37 |
Park and Chung |
|
Nurse |
GICC |
3.37±0.35 |
Son et al. (2013) |
|
Doctor, Nurse, |
GICC |
3.37±0.35 |
Lee and Kim (2010) |
|
Nurse, Doctor |
GICC |
3.37±0.45 |
Lee and Kim (2017) |
|
Nurse, Doctor |
ICU Nurse-Physician |
Openness (Nurse-Physician) 3.18±0.66 |
Cho
et al. (2013) |
|
Doctor, Nurse |
ICU Nurse-Physician |
Openness 2.76±0.82 Accuracy 2.74±0.72 Mutual understanding Timeliness 3.70±0.52 |
Yoo (2022) |
|
Nurse |
Communication Type |
Upward 3.27±0.39 |
Seo et al. (2003) |
|
Doctor, Nurse, |
Communication
Type |
Formal 2.97±0.30 |
Lee and Kim (2010) |
|
Nurse |
Nurse's Communication |
3.50±0.53* |
Koo and Kim (2014) |
|
Nurse, Doctor |
Tools to measure nurses' |
3.64±0.32 |
Yoon et al. (2018) |
|
Note *:
reverse question, GICC: Global Interpersonal Communication Competence |
|||
Table 9와 같이 중환자실에서 사용빈도가 높은 의사소통 측정도구는 글로벌 인간관계 의사소통능력 측정도구(GICC)가 4편으로 가장 높게 나타났고, ICU Nurse-Physician Questionnaire의 의사소통 도구 2편, 의사소통 유형 측정도구 2편, 간호사의 의사소통갈등 측정도구 1편, 간호사의 조직 내 의사소통 측정도구 1편 순으로 나타났다. 의사소통 대상은 간호사가 10편으로 가장 높게 나타났고, 의사 6편, 환자 3편, 보호자 2편 순으로 나타났다. 중환자실 간호사의 의사소통 수준은 3.16~3.37점으로 나타났다. 또한, 비공식적인(2.40~2.51점) 의사소통보다 공식적인(2.97~3.27점) 의사소통 점수가 높게 나타났다. 개방성은 의사(3.18점)와의 의사소통보다 간호사(3.46점)와의 의사소통 점수가 높게 나타났다. 정확성도 의사(2.79점)와의 의사소통보다 간호사(3.01점)와의 의사소통 점수가 높게 나타났다. 간호사 간의 의사소통갈등 점수가 3.50점으로 나타났다. 간호사 조직 내의 의사소통 점수는 3.64점으로 나타났다.
3.2.9 Hospital
Table 10은 병원 전체의 의사소통 대상과 수준을 정리한 것이다.
|
Communication |
Measuring tool |
Level of communication |
Author (Year) |
|
Nurse |
GICC |
3.45±0.37 |
Shin et al. (2018) |
|
Nurse |
GICC |
3.60±0.48 |
Park and Yoo (2020) |
|
- |
GICC |
3.51±0.40 |
Kim et al. (2019) |
|
Patient,
Nurse |
GICC |
3.67±0.28 |
Kim et al. (2018a) |
|
Cancer
patient |
GICC |
3.59±0.43 |
Kim and Park (2022) |
|
- |
GICC |
3.58±0.46 |
Kang et al. (2018) |
|
Nurse |
GICC |
3.71±0.35 |
Kang and Eun (2018) |
|
Nurse |
GICC |
3.34±0.17 |
Im and Kim (2008) |
|
Patient |
GICC |
3.56±0.43 |
Han and Park (2019) |
|
Cancer
patient |
GICC |
3.70±0.42 |
Han and Kim (2022) |
|
- |
GICC |
3.37±0.38 |
Cho and Seo (2018) |
|
Nurse |
Nurse's Communication
Conflict |
3.51±0.42* |
Kang and Lee (2006) |
|
Nurse, Patient, |
Nurse's Communication
Conflict |
3.62±0.53* |
Oh and Choi (2018) |
|
Nurse, Doctor |
Tools to measure
nurses' |
3.20±0.40 |
Park and Lee (2018) |
|
Nurse |
Tools to measure
nurses' |
3.05±0.44 |
Kim and Kim (2016) |
|
Nurse,
Patient |
Primary Communication Inventory (PCI) |
3.44±0.35 |
Jung and Shin (2011) |
|
Doctor |
Communication Type
Measurement Tool |
Upward 2.64±0.60 Downward 3.41±0.55 Horizontal 3.15±0.56 Informal 2.76±0.62 |
Kim et al. (2004) |
|
Nurse |
Tools to measure
nurses' |
3.38±0.44 |
Park and Lee (2011) |
|
- |
A communication
skills measurement tool |
3.80±0.44 |
Ahn (2017) |
|
Nurse,
Patient |
Communication Training Needs Questionnaire |
3.09±0.47 |
Hyeon (2002) |
|
Nurse, Doctor |
Life Skills
Assessment Tool: |
3.41±0.52 |
Yune et al. (2018) |
|
Nurse,
Patient |
Communication Skills Scale |
3.21±0.25 |
Kim et al. (2016) |
|
Nurse,
Patient |
Communication Skills Diagnostic Tool |
3.14±0.35 |
Ha and Jeon (2016) |
|
Nurse,
Patient |
Tools for communication disorder factors |
3.39±0.45 |
Kim et al. (2017) |
|
Note *: reverse question, GICC: Global Interpersonal Communication Competence |
|||
Table 10과 같이 병원 전체에서 사용빈도가 높은 의사소통 측정도구는 글로벌 인간관계 의사소통능력 측정도구(GICC)가 11편으로 가장 높게 나타났고, 간호사의 의사소통갈등 측정도구, 간호사의 조직 내 의사소통 측정도구 각 2편으로 나타났으며, 그 외에 Primary Communication Inventory (PCI), 의사소통 유형 측정도구, 간호사의 의사소통 유형 측정도구, 언어적 및 비언어적 의사소통 측정도구, 의사소통 훈련 요구 측정도구, 생애능력 측정도구(주도적 의사소통), 의사소통 척도 측정도구, 의사소통능력진단 도구, 의사소통장애요인 측정도구가 각 1편씩 다양한 측정도구가 활용되었다. 의사소통 대상은 간호사가 16편으로 가장 높게 나타났고, 환자 7편, 의사 3편, 암환자 2편, 보건의료종사자 1편 순으로 나타났다. 병원 전체 간호사의 의사소통 수준은 2.76~3.80점으로 나타났다. 간호사 간의 의사소통갈등 점수가 3.51~3.62점으로 나타났다. 간호사 조직 내의 의사소통 점수는 3.05~3.20점으로 나타났다.
3.3 Factors Affecting Communication and Strategies for Enhancement
Table 11, 12는 의사소통 영향요인 및 향상방안은 총 60편 논문 중에서 의사소통에 영향을 미치는 요인과 의사소통 향상방안이 모두 제시된 논문 44편을 대상으로 의사소통 영향요인 및 향상방안을 정리하였다.
Influence
factor |
Improvement plan |
Author (Year) |
|
Working |
Development of educational programs
to |
Kang and Jung (2019); Oh and Choi
(2018); Son et al. (2013); Cho et al. (2013) |
|
The need to establish a horizontal
and effective |
Son et al. (2013) |
|
|
Need to communication training |
Kim and Park (2022); Yoo (2022); Nam |
|
|
Activate informal organizations such
as small |
Lim and Yi (2014); Lee and Kim (2010) |
|
|
Operate
mentoring system, workshops, outings |
Lim
and Yi (2014) |
|
|
Operation of educational programs for
communication |
Lee and Kang (2018); Oh and Choi
(2018); |
|
|
Work (Clinical) |
Operation of communication training
programs |
Yoo (2022); Ahn (2017); Lee and Kim
(2017); |
|
Operate a communication skills
training program for |
Lee et al. (2013) |
|
|
Implementing a communication skills
enhancement program for low-year nurses |
Cho and Seo (2018); Son and Sung
(2017); |
|
|
Assertion
training program operation |
Kang
and Lee (2006) |
|
|
Operation of educational programs for
communication |
Lee and Kang (2018) |
|
|
Development and operation of
communication |
Cho et al. (2013) |
|
|
Communicative training programs
include groups |
Kim and Kim (2016) |
|
|
Communication |
Operation
of educational programs for communication |
Park
and Lee (2018); Shin (2018) |
|
Need
to develop communication media |
Han
and Kim (2022); Park and Lee (2018) |
|
|
Provide opportunities for reflection
through feedback |
Han and Kim (2022) |
|
|
Providing a means to share key information
about the |
Go et al. (2022) |
|
|
Use of various communication media
and deliver |
Yoon et al. (2018) |
|
|
Creating a horizontal communication atmosphere |
Kim et al. (2004) |
|
|
Experiencing |
Need attention to environmental
factors and |
Kim et al. (2017) |
|
Operate horizontal and open
communication training |
Jung et al. (2020) |
|
|
Shift system |
Need an educational program to
improve |
Han (2019) |
|
Development and operation of
communication |
Cho et al. (2013) |
|
|
Development of educational programs
that utilize |
Ha and Jeon (2016) |
Influence factor |
Improvement plan |
Author (Year) |
|
Relationship |
Develop interventions to practice effective communication between
healthcare providers |
Lee and Ji (2021) |
|
Moderation techniques, attempt to access the reflux |
Jeong et al. (2012) |
|
|
Operation of interpersonal
improvement programs |
Jung and Shin (2011) |
|
|
Organization |
Implementation of communication skills |
Kim et al. (2019) |
|
Develop interventions to practice effective |
Lee and Ji (2021) |
|
|
Health problem |
Coping with stress, operation
of mental health programs |
Jeong and Kim (2009) |
|
Create a horizontal atmosphere, implement an open |
Kim and Cho (2021) |
|
|
Create an organizational atmosphere that can relieve |
Jung et al. (2020) |
|
|
Experiences of |
Empathy from the other person's point of view, |
Jeoung et al. (2014) |
|
Reaction |
Operation of communication
training programs |
Im and Kim (2008) |
|
Concreteness, |
Operation of facilitated communication |
Park and Yang (2008) |
|
Resilience |
Operate specialized
programs to increase resilience |
Jung et al. (2020) |
|
Communication |
Operation of competency education programs to |
Kim and Lee (2019) |
Table 11, 12와 같이 영향요인은 작업부서, 근속년수(임상경력), 의사소통유형, 직장 내 폭력경험, 교대시스템(근무조 간의 인수인계), 동료 또는 환자와의 관계, 조직관리, 건강문제, 반응, 구체성 및 즉각성, 회복탄력성, 의사소통 효율성으로 나타났다.
각 영향요인에 대한 향상방안은 다음과 같다. 작업부서에 대한 향상방안으로는 의사소통 기술에 대한 교육프로그램 개발과 의사소통 훈련, 비공식 조직 활성화, 멘토링시스템, 워크샵 개최 등의 개선방안이 도출되었다. 근속년수(임상경력)에 따른 향상방안으로는 의사소통 향상 프로그램 운영, 저년차 또는 중간연차를 위한 의사소통 훈련 프로그램 등이 도출되었다. 의사소통 유형에 따른 향상방안으로는 의사소통을 위한 교육프로그램 운영, 의사소통 매체(수단)의 개발 필요, 피드백을 통하여 반영하는 기회 제공 등이 도출되었다. 또한 직장 내 폭력경험에 따른 향상방안으로 조직구성원 내에 수평적이고, 개방적인 의사소통 훈련 프로그램 제공 등이 나타났다. 교대시스템(근무조 간의 인수인계)는 의사소통 향상을 위한 교육프로그램 운영, 작업특성에 맞는 의사소통 시스템 개발 및 운영 등이 도출되었다. 동료 또는 환자와의 관계는 보건의료종사자 간의 효과적인 의사소통을 연습하기 위한 중재 개발, 대인관계 개선 프로그램 운영 등이 도출되었다. 조직관리는 의사소통 기술 훈련 프로그램 시행, 보건의료종사자 간의 효과적인 의사소통을 연습하기 위한 중재 개발, 의사소통 기술 훈련 프로그램 시행 등이 도출되었다. 건강문제에 대한 방안으로는 스트레스 대처, 정신건강 프로그램 운영, 수평적 분위기 조성, 열린 의사소통 프로그램 구현, 마음관리 프로그램 적용, 직무스트레스를 해소할 수 있는 조직적인 분위기 조성 등이 도출되었다. 의사소통 경험에서는 상대방 입장에서 공감, 상사에 대한 정확한 의사표현, 반응은 의사소통 교육 프로그램 운영 등이 나타났으며, 구체성과 즉각성은 의사소통 촉진 교육프로그램 운영 등이 도출되었다. 회복탄력성에 대한 향상방안으로는 회복탄력성 향상을 위한 특별프로그램 운영 등과 의사소통 효율성은 의사소통 효율성 제고를 위한 역량교육 프로그램 운영이 도출되었다,
본 연구에서는 간호사의 의사소통 도구와 의사소통 대상 및 수준, 의사소통 영향요인과 향상방안에 대해서 체계적인 문헌고찰을 실시하였다. 의사소통 수준을 측정하기 위하여 가장 많이 사용하는 측정도구는 글로벌 인간관계 의사소통능력 측정도구(GICC)가 가장 많이 사용되었고, 간호사의 조직 내 의사소통 측정도구, 의사소통 유형 측정도구, 간호사의 의사소통갈등 측정도구, ICU Nurse-Physician Questionnaire의 의사소통 도구가 주로 사용되었다. 의사소통 대상은 간호사가 가장 많았고, 의사, 환자, 보호자, 보건의료종사자 순으로 나타났다. 한편, 중환자실에서 간호사 간의 의사소통을 통한 건강한 작업환경을 파악하기 위해서 ICU Nurse-Physical Questionnaire를 사용하였다(Manojlovich and DeCicco, 2007).
의사소통 수준은 기타병동이 3.63점으로 가장 높았고, 수술실 3.58점, 내과병동 3.54점, 내외과병동과 병원 전체가 각각 3.53점, 외과 3.48점, 외래 3.47점, 중환자실 3.27점, 응급실 3.1점으로 나타났다. 문헌연구에 따르면 중환자실과 응급실의 특성상 무의식인 경우와 기계적 장치에 의한 호흡을 하는 환자가 많아 중환자실과 응급실 간호사들이 환자와 의사소통의 기회가 적고, 보호자와의 의사소통 기회 또한 중환자실 및 응급실 면회제한 등의 규정으로 인하여 의사소통을 할 기회가 줄어든다고 하였다(Son et al., 2013; Dingley et al., 2008; Pronovost et al., 2003). 따라서 중환자실과 응급실에 종사하는 간호사에 대해서 의사소통 수준을 높일 수 있도록 관리가 필요함을 알 수 있다.
대부분의 부서에서는 공식적인 의사소통보다 비공식적인 의사소통에 대한 의사소통 점수가 낮게 나타났다. 비공식적인 의사소통에 대한 의사소통 수준을 높일 수 있도록 관리가 필요함을 알 수가 있다. 의사소통 갈등 점수는 병원전체가 3.57점으로 가장 높았고, 내외과병동과 응급실, 중환자실이 각각 3.50점, 기타병동 3.32점으로 나타났다. 내외과병동과 응급실, 중환자실에 근무하는 간호사의 의사소통갈등 점수가 높아 갈등을 해결할 수 있는 개선방안이 필요함을 알 수 있다.
간호사 조직 내의 의사소통은 중환자실이 3.64점으로 가장 높게 나타났고, 내과병동 3.28점, 내외과병동 3.27점, 외과병동 3.23점, 응급실 3.21점, 수술실 3.18점, 병원 전체 3.13점 순으로 나타났다. 의사와 간호사 간의 의사를 보좌하는 수직적인 관계, 간호사 간의 수직적인 상하관계의 경직성도 의사소통에 대한 인식에 영향을 준다고 하였으며, 이러한 경직성은 의사소통의 차단과 과도한 긴장으로 이어진다고 하였다(Kim and Kim, 2016; Manser, 2009; Ummenhofer et al., 2001). 수술실에 근무하는 간호사가 간호사 조직 내의 의사소통 점수를 높일 수 있도록 개선방안이 필요함을 알 수 있다
의사소통 영향요인은 작업부서, 의사소통 유형, 직장 내 폭력경험, 교대시스템, 동료 및 환자와 관계, 조직관리, 건강문제, 의사소통 경험, 반응, 구체성과 즉각성, 회복탄력성, 의사소통 효율성으로 나타났다. 한편 교육 수준과 임금이 높은 간호사 사이에서 인지된 존중과 의사소통 만족도에서 평균 점수가 더 높다고 하였다(Hailu et al., 2016; Tschannen and Lee, 2012). 미국에서 수행된 연구에서 나온 결과는 개인의 업무 태도와 조직적 요인이 의사소통의 특성에 영향을 미친다고 하였다(Hailu et al., 2016; Sutcliffe et al., 2004).
의사소통 개선방안은 교육프로그램(의사소통 훈련, 의사소통 향상), 의사소통 매체(수단) 개발, 작업특성에 맞는 의사소통 개발, 수평적 분위기 조성, 상사에 대한 정확한 의사표현, 비공식조직 활성화 등 의사소통을 높일 수 있는 방안이 도출되었다. 수술 전 업무회의 같이 각 임상상황에 적합하게 개발된 표준화된 의사소통 도구를 활용함으로써, 직종 간의 차이를 극복하고 객관적이고 정확한 의사소통을 할 수 있다고 하였다(Kim and Kim, 2016; Lingard et al., 2006). 또한, 의료기관에서의 의사소통을 개선하기 위해서는 보건의료종사자 간의 상대방의 입장에서 생각하는 동시에, 간호사 내 상하관계의 유연한 의사소통이 될 수 있도록 중재가 이루어져야 하며, 병동 및 부서단위의 관리감독자가 함께하는 의사소통 프로그램으로 이루어져야 한다고 하였다(Kim and Kim, 2016; Pronovost et al., 2006). 또한, 의사소통 능력을 기르기 위해서는 의사와 간호사 또는 간호사와 다른 의료 직종 간의 협력 학습 및 의사 결정 기회를 통합하는 프로그램과 커리큘럼을 개발해야 한다고 하였다(Tschannen and Lee, 2012; American Association of Colleges of Nursing, 1995).
본 연구에서는 간호사의 의사소통 수준과 의사소통 대상, 의사소통의 영향요인과 개선방안에 대한 체계적 문헌고찰을 수행하였다. 간호사의 의사소통 수준을 측정하기 위하여 가장 많이 사용되는 도구는 글로벌 인간관계 의사소통능력 측정도구(Global Interpersonal Communication Competence, GICC)가 가장 많이 사용되었다. 본 연구에서 확인된 바와 같이 간호사의 의사소통 수준은 중환자실과 응급실에서 낮게 나타났으며, 의사소통 갈등은 내외과병동, 중환자실 및 응급실에서 높게 나타났다. 이러한 결과를 토대로 중환자실과 응급실, 내외과병동에서 근무하는 간호사들을 대상으로 의사소통 수준 향상 및 의사소통 갈등 해소를 위한 교육 프로그램이 필요한 것으로 사료된다. 또한, 1-6차까지 한국인 근로환경조사 문항(OSHRI, 2022)을 살펴본 결과 의사소통을 관련 문항이 포함되지 않았으므로, 향후 조사에서는 의사소통 관련 항목을 추가하여 진행하는 것을 제안하고자 한다.
본 연구는 간호사의 의사소통 특성을 파악하고 근로환경을 개선하기 위한 기초 자료를 제공하는 역할을 하였습니다. 또한, 간호사의 의사소통 문제가 심각하게 나타났으므로, 의사소통 능력을 향상시키고 지원하기 위한 노력이 필요하며, 이를 통해 간호사의 근로환경과 건강을 증진시킬 수 있을 것으로 기대한다.
References
1. Ahn, S.Y., The Convergence Relation of Communication, Emotional Labor, and Organizational Commitment among Nurse, Journal of the Korea Convergence Society, 8(6), 147-152, 2017. https://doi.org/10.15207/JKCS.2017.8.6.147
Google Scholar
2. American Association of Colleges of Nursing, AACN position paper: interdisciplinary education and practice; March, 1995.
3. An, S.A., Ham, S.H., Lee, W.H., Choi, W.J. and Kang, S.K., Occupational Diseases among Health Workers, Journal of Korean Society of Occupational and Environmental Hygiene, 30(4), 353-363, 2020. https://doi.org/10.15269/JKSOEH.2020.30.4.353
4. Brown, J.B., Lewis, L., Ellis, K., Stewart, M., Freeman, T.R. and Kasperski, M.J., Mechanisms for communicating within primary health care teams. Canadian Family physician Medecin de famille canadien, 55(12), 1216-1222, 2009.
5. Cho, J. and Seo, K., Influence of Communication competence and Compassion competence on Resilience of Clinical Nurse, Journal of the Korean Society for Wellness, 13(4), 51-60, 2018.
6. Cho, Y.A., Kim, M.K., Cho, M.S. and Nam, E.Y., Nurses' Communications with Health Professionals, Journal of Korean Clinical Nursing Research, 19(1), 20-32, 2013.
7. Dingley, C., Daugherty, K., Derieg, M.K. and Persing, R., Improving Patient Safety Through Provider Communication Strategy Enhancements. In: Henriksen K, Battles JB, Keyes MA, et al., editors. Advances in Patient Safety: New Directions and Alternative Approaches (Vol. 3: Performance and Tools). Rockville (MD): Agency for Healthcare Research and Quality, 2008. Available from: https://www.ncbi.nlm.nih.gov/books/NBK43663/
Google Scholar
8. Go, Y.J., Lee, M.H. and Kim, M.Y., The Effect of Hospital Internal Marketing and Organizational Communication Perceived by Nurses on Organizational Performance, Journal of Digital Convergence, 20(2), 479-486, 2022.
9. Ha, J.Y. and Jeon, S.Y., The Effects of Humanistic Knowledge and Emotional Intelligence on Communication Skills of Nurses, The Journal of Korean Academic Society of Nursing Education, 22(3), 264-273, 2016.
Google Scholar
10. Hailu, F.B., Kassahun, C.W. and Kerie, M.W., Perceived Nurse-Physician Communication in Patient Care and Associated Factors in Public Hospitals of Jimma Zone, South West Ethiopia: Cross Sectional Study. PloS One, 11(9), e0162264, 2016. https://doi.org/ 10.1371/journal.pone.0162264
Google Scholar
11. Han, M.J. and Kim, S., Effects of Compassionate Competence, Communication Skills, and Nursing Work Environment on Person-centered Care in General Hospital Nurses who Care for Cancer Patients, The Korean Journal of Rehabilitation Nursing, 25(1), 11-21, 2022.
Google Scholar
12. Han, S.H., Effecting Factors Job Satisfaction of nurses, The Convergent Research Society Among Humanities, Sociology, Science, and Technology, 9(11), 799-808, 2019.
13. Han, S.M. and Park, S.J., The Effects of Communication Skill and Job Stress on Organizational Effectiveness of Geriatric Hospital Nurses, Nursing & Health Issues, 24(2), 124-132, 2019.
14. Hyeon, M.Y., The Communication Training Needs of Nurses in the University Hospital, Journal of Korean Academy of Psychiatric Mental Health Nursing, 11(4), 443, 2002.
15. Im, S. and Kim, E.K., Interpersonal Communication Competence and Difficult Communication Experiences of Preceptor Nurses, Journal of Korean Academy of Psychiatric and Mental Health Nursing, 17(4), 471-480, 2008.
16. Jeong, H.S., Choi, S.E. and Kim, S.D., Relationship between Nurse Managers' Facilitative Communication and Nurses' Self-esteem, Korean Journal of Occupational Health Nursing, 21(3), 175-183, 2012.
Google Scholar
17. Jeong, S.J. and Kim, K.H., Empathy Ability, Communication Ability, and Nursing Performance of Registered Nurses and Nursing Assistants in Long-term Care Hospitals, Journal of Korean Academy of Nursing Administration, 23(3), 249-258, 2017.
Google Scholar
18. Jeong, S.J. and Kim, S.J., The Relationship of Communication Types, Interpersonal Relations and Depression for Nurses in Hospital Setting, Nursing & Health Issues, 14(1), 1-20, 2009.
19. Jeoung, Y.O., Park, S.C., Jin, J.K., Kim, J.Y., Lee, J.U., Park, S.Y. and Sok, S., Content analysis of communication between nurses during preceptorship, Journal of Korean Academy of Psychiatric and Mental Health Nursing, 23(2), 82-92, 2014. https:// doi.org/10.12934/jkpmhn.2014.23.2.82
Google Scholar
20. Jung, E.H., The Effect of Positive Psychological Capital on the Communication Competence and Job Satisfaction of Geriatric Hospital Nurses, Journal of the Korea Entertainment Industry Association, 13(1), 235-243, 2019.
21. Jung, H.J., Lee, Y.S. and Shin, S.H., A Study the Relationships among Verbal Violence Experience, Job Stress, and Resilience and the Communication Ability of Operating Room Nurses, Journal of Korean Academy of Nursing Administration, 26(2), 120-129, 2020.
22. Jung, G.H. and Shin, S.H., Affecting Factors of Nurses' Communication, Journal of East-West Nursing Research, 17(2), 164-170, 2011. https://doi.org/10.14370/JEWNR.2011.17.2.164
23. Kang, H.S. and Kim, Y.Y., Influence of the Emotional Intelligence, Communication Competence and Stress coping on Turnover Intention in Psychiatric Nurses, Journal of the Korea Academia-Industrial Cooperation Society, 17(1), 141-151, 2016.
Google Scholar
24. Kang, M.J. and Lee, H., The Effect of Assertiveness Training on Communication Related Factors and Personnel Turnover Rate among Hospital Nurses, Journal of Korean Academy of Nursing, 36(5), 681-690, 2006.
Google Scholar
25. Kang, Y.S., Kwon, Y.C. and Kim, Y., The Effect of Communication Competency and Job Stress of Long Term Care Hospital Nurses on Turnover Intention focused on control effect of emotional intelligence, Journal of Digital Convergence, 16(12), 449-457, 2018. https://doi.org/10.14400/JDC.2018.16.12.449
26. Kang, Y.J. and Jung, K.I., Effects of Emotional Intelligence and Nursing Working Environment on Nursing Performance of Nurses Caring for Cancer Patients in Small and Medium Hospitals: The Mediating Effect of Communication Competence, Asian Oncology Nursing, 19(4), 233-241, 2019.
27. Kang, Y.M. and Eun, Y., The Effects of Self-efficacy, Critical Thinking Disposition, Self-leadership, and Communication Competency on the Core Competencies of the Preceptor in Advanced General Hospitals, The Journal of Korean Academic Society of Nursing Education, 24(3), 279-289, 2018.
Google Scholar
28. Kim, B.J., Lee, S.Y., An, G.J., Lee, G. and Yun, H.J., Influence of Communication Competency and Nursing Work Environment on Job Satisfaction in Hospital Nurses, Journal of Health Informatics and Statistics, 44(2), 189-197, 2019.
29. Kim, C.S., Lee, M.O. and Lee, S.B., Effects of Nonviolent Communication(NVC) Program consist of Communication Competency, Communication Self-Efficacy and Stress in Nurses, Health Service Management Review, 10(3), 9-17, 2016.
30. Kim, H.J. and Park, J.S., Effect of Emotional Intelligence, Job Stress, and Communication Ability on Nursing Performance of Nurses Caring for Cancer Patients, Journal of East-West Nursing Research, 28(1), 57-66, 2022.
Google Scholar
31. Kim, J.W., Kim, K.H, Chung, H.K. and Kwak, Y.H., The Influence of Communication Barriers on Nursing Performance of Intensive Care Units Nurses, Journal of the Korean Society for Wellness, 12(1), 45-56, 2017.
32. Kim, K.H. and Lee, J.E., Factors Influencing Nurses' Job Satisfaction in Integrated Nursing and Care Services Unit: Focused on Compassion Fatigue, Compassion Satisfaction and Communication Efficacy, The Korean Journal of Rehabilitation Nursing, 22(2), 124-133, 2019.
33. Kim, K.I., Kim, S.J. and Kim, B.Y., A Convergence Study about the Effects of Assertiveness Training on Nurses' Fear of Negative Evaluation, Assertiveness Behavior, and Communication Competency, Journal of the Korea Convergence Society, 9(10), 487-495, 2018a.
Google Scholar
34. Kim, K.O., Ko, M.S., Choi, E.H. and Kim, H.J., A Comparative Study on Communication in Competence, Nursing Professionalism, Work Environment and Job Satisfaction between Outpatient Nurses and Ward Nurses, Health Communication, 13(2), 175-183, 2018b.
35. Kim, M.J. and Kim, K.J., The influence of nurses' clinical career and communication within organization on teamwork competency, Journal of Digital Convergence, 14(2), 333-344, 2016.
Google Scholar
36. Kim, N.K. and Cho, G.Y., Correlation between Conflict Management Style, Communication Competence and Burnout in Operating Room Nurses, Journal of The Korean Data Analysis Society, 23(2), 771-786, 2021.
37. Kim, S.H. and Lee, M.A., Effects of Emotional Labor and Communication Competence on Turnover Intention in Nurses, Journal of Korean Academy of Nursing Administration, 20(3), 332-341, 2014.
Google Scholar
38. Kim, S.K., Organization and human behavior. Seoul: MunKyungsa, 2005.
39. Kim, S. and Yang, J., The Effects of Motivational Interviewing Training Program on Communication Skills and Self-Efficacy of Home Visiting Nurses, Journal of Korean Public Health Nursing, 30(2), 274-287, 2016.
Google Scholar
40. Kim, Y.S., Park, J.W., Park, J.H., Lee, S.M. and Lim, K.Y., A Comparison of the Awareness of Medical Residents' Power Style, Communication Type and Organizaitional Effectiveness in Nurses and Technologists, Korean Journal of Medical Education, 16(3), 309-318, 2004.
Google Scholar
41. Koo, M.J. and Kim, K.N., A Study on the Development and Evaluation of Hospital Communication (Hospital Adaptation) Program for New Graduate Nurses, The Korean Journal of Health Service Management, 8(4), 1-12, 2014.
Google Scholar
42. Lee, A.K., Yeo, J.Y., Jung, S. and Byun, S.S., Relations on communication competence, job-stress and job-satisfaction of clinical nurse, The Journal of the Korea Contents Association, 13(12), 299-308, 2013.
Google Scholar
43. Lee, E.K. and Kim, O.H., Collaboration between Nurse- Doctor and Interpersonal Communication Competence of Nurse, Health Communication, the Official Journal of Korean Academy on Communication in Healthcare, 4(1), 49-57, 2009.
44. Lee, G.M. and Ji, E.S., The Influence of Nurses' Organizational Communication and Self-Leadership on Patient Safety Competence in Comprehensive Nursing Service Units: Focusing on Small and Medium-sized Hospitals, Journal of East-West Nursing Research, 27(2), 114-123, 2021.
Google Scholar
45. Lee, H.S. and Kim, J.K., Relationship among Communication Competence, Communication Types, and Organizational Commitment in Hospital Nurses, Journal of Korean Academy of Nursing Administration, 16(4), 488-496, 2010.
Google Scholar
46. Lee, I.S. and Kim, C.H., Conflict Management Style, Communication Competence, and Collaboration among Hospital Nurses and Physicians, The Korean Journal of Rehabilitation Nursing, 20(1), 69-78, 2017.
Google Scholar
47. Lee, J. and Gang, M., Factors Influencing the Communication Behavior of nurses caring for people with Dementia - Focused on the compassionate competence and Burnout -, Journal of the Korea Academia-Industrial Cooperation Society, 19(10), 498-505, 2018.
Google Scholar
48. Lee, M.O. and Lee, S.B., Effects of Nonviolent Communication(NVC) Program consist of Communication Ability, Relationship and Anger in Nurses, Journal of the Korea Society of Computer and Information, 21(10), 85-89, 2016.
49. Lim, E.J. and Yi, Y.J., Comparison of Operating Room Nurses and General Ward Nurses on Communicative Competence and Interpersonal Relationship Ability within the Medical Team, Journal of Korean Academy of Nursing Administration, 20(3), 313-321, 2014.
Google Scholar
50. Lingard, L., Whyte, S., Espin, S., Ross Baker, G., Orser, B. and Doran, D., Towards safer interprofessional communication: constructing a model of "utility" from preoperative team briefings, Journal of Interprofessional Care, 20(5), 471-483, 2006.
Google Scholar
51. Manser, T., Teamwork and patient safety in dynamic domains of healthcare: a review of the literature. Acta Anaesthesiologica Scandinavica, 53(2), 143-151, 2009.
Google Scholar
52. Manojlovich, M. and DeCicco, B., Healthy work environments, nurse-physician communication, and patients' outcomes. American journal of critical care: an official publication, American Association of Critical-Care Nurses, 16(6), 536-543, 2007.
53. Mathis, R.L. and Jackson, J.H., Human resource management. Cincinnati: South-Western College Publication, 2010.
54. Moher, D., Liberati, A., Tetzlaff, J. and Altman, D.G., PRISMA Group, Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement, PLoS Medicine, 6(7), e1000097, 2009.
Google Scholar
55. Nam, H.R., Lee, E. and Heo, H.S., Effects of Emotional Labor and Communication Competence on Geriatric Nursing-related Stress in Nurses Caring for Older Patients, Korean Journal of Occupational Health Nursing, 29(1), 20-28, 2020.
Google Scholar
56. Oh, E.J. and Choi, H.K., Comparison of Psychiatric and Clinical Nurses on Emotional Intelligence, Facilitative communication ability and Communication Conflicts, Journal of Digital Convergence, 16(5), 329-340. 2018.
Google Scholar
57. Oh, E.J., Lee, M.H. and Ko, S.H., Influence of Emotional Intelligence and Empathy on the Facilitative Communication Ability of Psychiatric Nurses, The Korean Academy of Psychiatric and Mental Health Nursing, 25(4), 283-293, 2016.
Google Scholar
58. OSHRI, 6th Korean Working Conditions Survey (2020), 2022. http://oshri.kosha.or.kr/eoshri/resources/KWCSDownload.do (retrieved May 6, 2022).
59. Park, E.J. and Lee, Y.M., Effect of Professional Autonomy, Communication Satisfaction, and Resilience on the Job Satisfaction of Intensive Care Unit Nurses, Korean Society of Critical Care Nursing, 11(2), 63-74, 2018.
Google Scholar
60. Park, H.M. and Lee, H.S., A Study of Communication Style, Critical Thinking Disposition, Job Satisfaction and Job Stress in Hospital Nurses, Perspectives in Nursing Science, 8(2), 105-112, 2011.
Google Scholar
61. Park, J.H. and Chung, S.K., Influence of Emotional Labor, Communication Competence and Resilience on Nursing Performance in University Hospital Nurses, Journal of the Korea Academia-Industrial Cooperation Society, 17(10), 236-244, 2016.
Google Scholar
62. Park, S.Y., Influences of Professional Autonomy, Communication Competency on Job Satisfaction of Psychiatric Nurses, Journal of Korean Academic Society of Home Health Care Nursing, 25(3), 232-239, 2018.
63. Park, S.Y. and Yoo, J.S., Factors Influencing Organizational Commitment of Nurses in Korean Red Cross Blood Center: Focusing on Positive Psychological Capital, Communication Ability, and Social Support, Research in Community and Public Health Nursing, 31(2), 179-188, 2020.
Google Scholar
64. Park, Y.R. and Yang, S., Nurse Managers' Facilitative Communication and Nurses' Organizational Commitment, Job Satisfaction, and Empowerment, Journal of Korean Academy of Psychiatric and Mental Health Nursing, 17(3), 342-352, 2008.
65. Pronovost, P., Berenholtz, S., Dorman, T., Lipsett, P.A., Simmonds, T. and Haraden, C., Improving communication in the ICU using daily goals, Journal of Critical Care, 18(2), 71-75, 2003. https://doi.org/10.1053/jcrc.2003.50008
Google Scholar
66. Pronovost, P.J., King, J., Holzmueller, C.G., Sawyer, M., Bivens, S., Michael, M., Haig, K., Paine, L., Moore, D. and Miller, M., A web-based tool for the Comprehensive Unit-based Safety Program (CUSP). Joint Commission Journal on Quality and Patient Safety, 32(3), 119-129, 2006. https://doi.org/10.1016/s1553-7250(06)32017-x
Google Scholar
67. Roberts, K.H. and O'Reilly, C.A., Measuring organizational communication, Journal of Applied Psychology, 59(3), 321-326, 1974. https://doi.org/10.1037/h0036660
68. Samur, M. and Intepeler, S.S., Factors influencing nurses' perceptions of occupational safety, Archives of Environmental & Occupational Health, 72(1), 45-52, 2017. https://doi.org/10.1080/19338244.2016.1156045
Google Scholar
69. Sutcliffe, K.M., Lewton, E. and Rosenthal, M.M., Communication failures: an insidious contributor to medical mishaps. Academic Medicine: Journal of the Association of American Medical Colleges, 79(2), 186-194, 2004. https://doi.org/10.1097/00001888-200402000-00019
70. Seo, E.A., Park, K.M. and Lee, B.S., Relations Between the Types of Communication and, Job Satisfaction and Nursing Performance in Staff Nurses, Journal of Korean Public Health Nursing, 17(2), 317-332, 2003.
71. Shin, N.Y., The Effect of Simulation-Based Training applying Situation-Background-Assessment-Recommendation (SBAR) on Nurse Shift Handover on Self Efficacy and Communication Skills in New Nurses, Journal of Korean Society for Simulation in Nursing, 6(2), 57-68, 2018.
72. Shin, Y., Lee, S., Moon, H., Jung, D. and Lee, H., Effects of Satir's model Based Communication Education on Communication Competence, Emotional Intelligence and Depression-happiness of Regional Public Hospital Nurses, Journal of Korean Public Health Nursing, 32(1),1 22-134, 2018
Google Scholar
73. Shortell, S.M., Rousseau, D.M., Gillies, R.R., Devers, K.J. and Simons, T.L., Organizational assessment in intensive care units (ICUs): construct development, reliability, and validity of the ICU nurse-physician questionnaire, Medical Care, 29(8), 709-726, 1991. https://doi.org/10.1097/00005650-199108000-00004.
74. Son, H.M., Sung, K.M., The Mediating Effects of Self-efficacy in the Relationship between Communicative Competence within the Medical team and Turnover Intention in Hospital Nurses. Journal of the Korea Academia-Industrial Cooperation Society, 18(12), 300-309, 2017.
75. Son, Y.J., Lee, Y.A., Sim, K.N., Kong, S.S. and Park, Y.S., Influence of Communication Competence and Burnout on Nursing Performance of Intensive Care Units Nurses, Journal of the Korean Academy of Fundamentals of Nursing, 20(3), 278-288, 2013. https://doi.org/ 10.7739/jkafn.2013.20.3.278
76. Statistics Korea, Korean standard classification of occupations (KSCO). 2017. [cited 2021 Mar 21]. Available from: http:// kssc.kostat.go.kr/ksscNew_web/ekssc/main/main.do# (retrieved Mar 21, 2021).
77. Tschannen, D. and Lee, E., The impact of nursing characteristics and the work environment on perceptions of communication, Nursing Research and Practice, 401905, 2012. https://doi.org/10.1155/2012/401905
78. Ummenhofer, W., Amsler, F., Sutter, P.M., Martina, B., Martin, J. and Scheidegger, D., Team performance in the emergency room: assessment of inter-disciplinary attitudes. Resuscitation, 49(1), 39-46, 2001. https://doi.org/10.1016/s0300-9572(00)00304-x
Google Scholar
79. Yoo, M.J., A Study on the Perception of Communication Between Doctors and Nurses in Advanced General Hospital, Journal of Industrial Convergence, 20(1), 77-86, 2022. https://doi.org/10.22678/jic.2022.20.1.077
Google Scholar
80. Yoon, S.H., Lee, T.W., Park, H.Y. and Song, Y.W., The Influence of Nurses' Emotional Intelligence and Communication within the Organization on Teamwork in Armed Forces Hospitals, Korean Journal of Occupational Health Nursing, 27(1), 67-75, 2018.
81. Yune, S.J., Lee, E.Y. and Park, K.H., Relationship between Communication, Interpersonal understanding, Proactivity in problem solving, and Team efficacy of Medical students and Nursing students, The Convergent Research Society Among Humanities, Sociology, Science, and Technology, 8(2), 369-378, 2018.
PIDS App ServiceClick here!