eISSN: 2093-8462 http://jesk.or.kr
Open Access, Peer-reviewed
eISSN: 2093-8462 http://jesk.or.kr
Open Access, Peer-reviewed
Xin Cui
, Ah Lam Lee
, Heeeun Kim
, Eunjin Jeon
, Chunlong Yu
, Heecheon You
10.5143/JESK.2023.42.4.289 Epub 2023 August 30
Abstract
Objective: The present study aims to provide a comprehensive review of the literature on fit evaluation methods for filtering facepiece respirators (FFRs) and identify research directions in future.
Background: Effective fit evaluation methods are needed for the design and certification of FFRs.
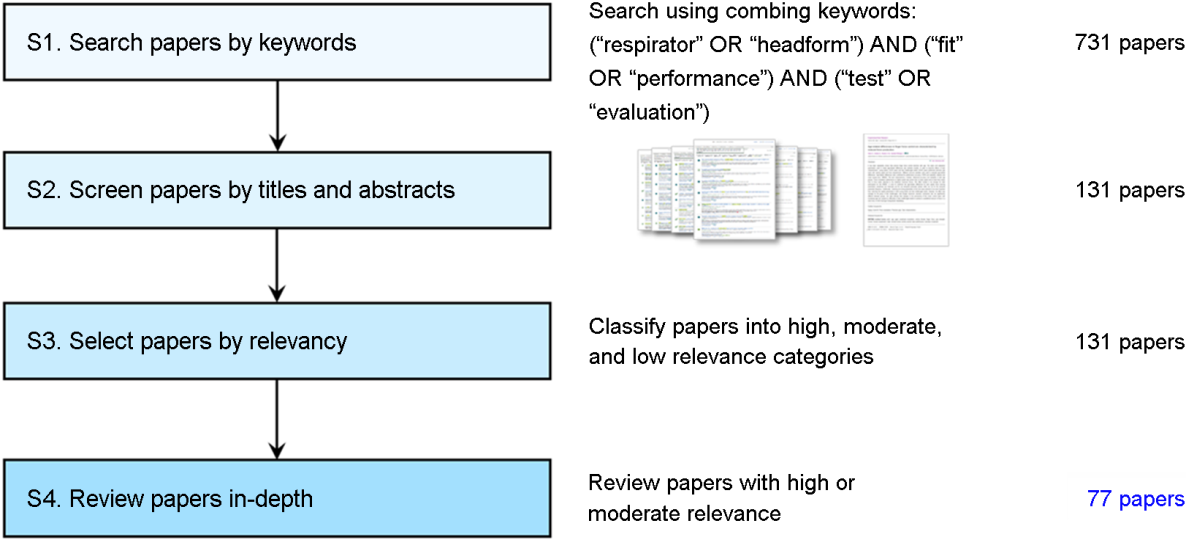
Method: A literature review was conducted on 77 papers selected as relevant to FFR fit evaluation by screening titles, abstracts, and full texts.
Results: Fit evaluation methods for FFRs were classified in the present study mainly into human-based and non-human based (using a headform or simulation) methods and their corresponding protocols and issues of validation were summarized accordingly. Furthermore, the positive and negative features of human-based and non-human based methods were compared in terms of convenience, cost-effectiveness, representativeness, and applicability.
Conclusion: Non-human based fit evaluation methods need to be developed because they are more convenient, cost-effective, representative, and applicable than human-based methods.
Application: This work provides comprehensive information on FFR fit evaluation methods and can guide the development of effective fit evaluation methods for various contexts.
Keywords
Facepiece filtering respirator Fit evaluation Fit testing Total inward leakage test Headform
An effective fit evaluation method during the design and certification stages of filtering facepiece respirator (FFR) is important to provide proper protection for the wearer from hazardous agents in various situations. FFRs have been used not only in industrial workplaces and medical fields but also in our daily living environments (Bergman et al., 2012; Ciotti et al., 2012; Park et al., 2021; Wardhan et al., 2020). An FFR design is evaluated to test compliance with regulatory requirements as well as to identify and resolve design problems such as air leakage, excessive pressure, and/or discomfort (Brosseau, 2010; Fakherpour et al., 2021; Karuppasamy and Obuchowski,2021; Lawrence et al., 2006; Manganyi et al., 2017; Or et al., 2016).
Human-based fit evaluation involves detecting the penetration of test agents through pathways between a face and an FFR while a body movement protocol is administered. Test agents can enter an FFR through the respiratory interface (RI), including face seal, filter element, exhalation valves, and other pathways (e.g., areas where head straps are connected to the FFR by staples and stitching (Bergman et al., 2015; Han and Lee, 2005; Jung and Lee, 2021; Rengasamy et al., 2014). The human-based fit evaluation methods are divided into total inward leakage (TIL), inward leakage (IL) test, and fit testing methods according to the detection area of leakage using test agents. The TIL test measures the leakage of the ambient atmosphere into the FFR through all pathways, while the IL test measures the leakage only through the RI. The IL test is usually considered the same as the TIL test because the leakage through other pathways is usually insignificant and can be ignored (Bergman et al., 2014; Clayton and Vaughan, 2005; Grinshpun et al., 2009; Han and Lee, 2005). Lastly, fit testing assesses the leakage of the face seal only, which is considered significant for respiratory protection (Bergman et al., 2014; Coffey et al., 1998; Coffey et al., 2012; Reponen et al., 2011; Rengasamy et al., 2018; Zhang et al., 2003). Note that both the TIL test and fit testing methods have been standardized in various countries. For example, fit testing is required in countries such as the United States, Canada, and Australia (CAN, 2018; Han, 2004; OSHA, 2021; OHS, 2020; WA Government, 2022), while TIL test regulations are used in Korea and European countries for FFR certification (Han, 2004; Han and Lee, 2005; Han, 2015; KFDA, 2019).
Non-human based fit evaluation methods have been developed to overcome the limitations of human-based fit evaluations. Human-based fit evaluations are limited by their use of non-hazardous agents such as sodium chloride, instead of actual health-related airborne particles like combustion aerosol or biological pathogens which pose health risks and raise ethical concerns (Bergman et al., 2015; He et al., 2014; Kim, 2016; Seo et al., 2020; Wander et al., 2012). Furthermore, human-based fit evaluations are expensive and time-demanding and only provide a general assessment of respirator performance without identifying specific unfit locations (Cui et al., 2022; Yang et al., 2009). To overcome these limitations, non-human-based fit evaluations using headforms or simulation techniques have been developed. For example, Kim (2016) used hazardous agents (silver nanoparticles) to investigate the fit of FFRs with a breathing machine and headforms, instead of non-hazardous agents. Next, Chu et al. (2015) improved the design of a respirator by evaluating the geometric similarity between the sealing curve of a digital respirator and its projected 3D curve on a face model using a virtual try-on system, which enhances the respirator's fit level before prototyping. Lastly, Lei et al. (2014) identified the unfit location of six FFRs by estimating the contact pressure between digital FFR models and a digital face through finite element analysis.
The present study aims to provide a comprehensive review of fit evaluation methods for FFRs to facilitate the design and development of experiments related to FFR fit evaluation. This review examines various human-based and non-human based fit evaluation methods, analyzing their positive and negative features. To the best of our knowledge, no reviews on fit evaluation methods for FFRs from both human and non-human perspectives have been conducted. Therefore, this review not only fills a significant gap in the existing literature but it also offers substantial academic and practical benefits by providing a consolidated analysis and overview of evaluation methodologies, thereby aiding in the advancement of research and practice in the area of respirator fit testing.
A total of 77 papers were screened in a systematic manner for an in-depth analysis of fit evaluation methods for FFRs using four steps: (1) paper search by keywords, (2) paper screening by titles and abstracts, (3) paper evaluation by relevancy, and (4) in-depth paper review (Figure 1). First, 731 papers published in English within the last 20 years were identified on Scopus and ScienceDirect using combining keywords of ("respirator" or "headform"), ("fit" or "performance"), and ("test" or "evaluation") on August 22, 2021. To ensure an expansive range of search results, the combining keywords were selected based on varying terms that shared similar thematic properties, which included the object of evaluation (respirator or headform), the measure of evaluation (fit or performance), and the concept of evaluation (test or evaluation). Second, three reviewers (two ergonomists and one clothing and textile expert) independently conducted a two-round screening by checking the titles and abstracts of the identified papers. Third, the screened papers were evaluated in terms of relevance (high, moderate, and low). Lastly, an in-depth review was conducted by checking the full text of 46 highly and 31 moderately relevant papers.
The fit evaluation methods were summarized into two main categories: human-based and non-human based fit evaluation methods (Table 1), and a comparison of the positive and negative features of these two methods was conducted in terms of convenience, cost-effectiveness, representativeness, and applicability.
3.1 Human-based fit evaluation
3.1.1 General requirements
General requirements for human-based fit evaluation are summarized in terms of participant recruitment and experiment procedures. The general requirements for participant recruitment include considerations such as health conditions, potential interference between a face and a respirator, and gender composition. Participants included in the fit evaluation should be in good health and able to wear respirators medically without diseases such as cardiovascular, high blood pressure, or respiratory diseases (Brosseau et al., 2010; Fakherpour et al., 2021; OSHA, 2021). To ensure a diverse range of face shapes is represented, fit test panels such as the NIOSH bivariate panel, the NIOSH PCA panel, or other panels for specific populations can be (Brosseau et al., 2010; Fakherpour et al., 2021; Grinshpun et al., 2021; Manganyi et al., 2017; Sietsema and Brosseau, 2018). To avoid interference with the respirator fit, participants with facial hair or certain facial characteristics should be excluded (Fakherpour et al., 2021; ISO 16975-3, 2017; Karuppasamy and Obuchowski, 2021; Sietsema and Brosseau, 2018). The general requirements for the experiment procedures, such as restrictions on activities and proper respirator wearing guidance, should be clearly communicated to participants before and during the experiment. For example, participants should be asked to refrain from smoking and eating for at least 30 or 60 minutes before the experiment (Foereland et al., 2019; Hauge et al., 2012). During the preparation stage, participants should also be instructed on the correct way to wear a respirator and conduct a seal check according to the manufacturer's instructions (Foereland et al., 2019).
3.1.2 Subjective and objective evaluation methods
In human-based subjective evaluation, the fit of an FFR is assessed through qualitative fit testing (QLFT) and comfort evaluation methods. The QLFT subjectively evaluates the fit of the FFR by determining if the participant can detect the taste of test aerosols, such as sodium saccharin, when breathing through the FFR (Fakherpour et al., 2019; OSHA, 2021; Pan et al., 2021; Wardhan et al., 2020). For example, Fakherpour et al. (2019) evaluated the fit of filtering respirators by using commercial and homemade BitrexTM (bitter taste) and sodium saccharin (sweet taste) aerosols. In addition, the comfort evaluation methods use a Likert scale or a visual analog scale (VAS) to evaluate the overall comfort of the respirator and/or its comfort in specific regions over an adequate period (Foereland et al., 2019; Karuppasamy and Obuchowski, 2021; OSHA 2021). For example, the Occupational Safety and Health Administration (OSHA) in the USA requires participants to wear the respirator for at least five minutes to assess its comfort level in terms of face regions (e.g., the mask on the nose, cheeks, and face) and rooms (e.g., room to talk) (OSHA 2021).
In human-based objective evaluation, the fit of an FFR is assessed through TIL test and quantitative fit testing (QNFT) methods. The TIL test measures the leakage between the FFR's protective barrier and a subject's face during a series of body movements (ISO 16975-3, 2017; ISO 16900-1, 2019). For example, the TIL test of Korean Standard measures leakage levels by calculating the concentration of test aerosol (e.g., sodium chloride) inside and outside the FFR, and the total duration of inhalation and exhalation while the subject performs daily activities on a treadmill (KFDA, 2019). The QNFT evaluates face seal leakage with a numerical indicator, the fit factor (FF), through two protocols: generated aerosol QNFT and ambient aerosol condensation nuclei-counting (CNC) QNFT. The generated aerosol QNFT method introduces a test aerosol (e.g., sodium chloride) into a fit-test chamber that surrounds the head and shoulders or the entire body of the subject and measures FF as the ratio of the aerosol outside and inside the respirator, while the ambient CNC QNFT collects and measures the ambient aerosols (ISO 16975-3, 2017).
Most human-based fit evaluation studies using accepted fit evaluation protocols do not assess the validity of their results, while others validate their methods through statistical comparison with reference fit evaluation protocols (ANSI/AIHA Z88.10, 2010; Coffey et al., 2002; Grinshpun et al., 2021; Hauge et al., 2012; Or et al., 2016; Rengasamy et al., 2014; Sreenath et al., 2001; Sietsema and Brosseau, 2016; Sun et al., 2019). For example, Fakherpour et al. (2021) evaluated the fit of commonly used FFRs during the COVID-19 pandemic using the OSHA QNFT protocol, but did not assess the validity of the results. In contrast, Grinshpun et al. (2021) validated a newly developed fit test protocol using the AccuFIT 9000 instrument (Kanomax-Japan Inc., Suita-city, Osaka, Japan) by comparing it with the US OSHA-accepted standard protocol with its sensitivity, specificity, and Kappa statistics. In addition, Coffey et al. (2002) evaluated the adequacy of five fit evaluation methods for N95 FFRs by comparing the correlation of their FFs with those of a simulated workplace protection factor (SWPF) protocol, which has a different set of exercises in terms of number and type.
3.2 Non-human based fit evaluation
3.2.1 Headform-based fit evaluation method
Static and robotic headforms have been developed to evaluate the fit of FFRs by simulating the facial features, breath patterns, dynamic movements, and sealing interactions during human-based fit evaluation experiments for a target population. An example of a static headform is the Static Advanced Headform (StAH), developed by NIOSH based on a medium-sized digital headform of the US workforce, which features a silicone polymer skin with defined local tissue thickness. The fit evaluations of N95 FFRs using the StAH were conducted with an experimental setup that included the StAH and a Breathing Recording System (Koken Ltd., Japan), which employed "normal breathing" and "deep breathing" patterns recorded from human subjects (Bergman et al., 2014; Bergman et al., 2015; Wander, 2012). In addition, static headforms that consider Korean facial features have been developed with skin textures that comply with material specifications (Seo et al., 2020). On the other hand, a humanlike robotic headform called Articulated Advanced Headform (ArtAH) was also developed by NOISH which developed to simulate head movements (turning the head side to side, and moving the head up and down) and speech via articulated structures (Wander, 2012). However, the fit testing experiment protocol using a robotic headform has not established yet (Wander, 2012).
Several non-human-based fit evaluation methods using static headforms have been validated through experiments, while those using robotic headforms still require further validation. The validity of non-human-based fit evaluation methods needs to statistically correlate to the human-based fit evaluation results, depending on how closely the headform simulates the human's facial features in terms of shape and material, breath pattern, dynamic movements and also sealing interaction between a respirator to face. For example, Bergman et al. (2014) validated that the shape difference of the face area of StAH was acceptable (1~2mm), and only a minor difference (< 1mm) in the face area was found after conducting 112 fit testings. Furthermore, a strong correlation (R2 = 0.95) of FF and a low difference in passing rate (<20%) were found between the StAH and human subjects (n = 10) during fit test experiments, which suggests that the StAH may serve as an alternative to human test subjects for certain respirator models (Bergman et al., 2015). Bałazy et al. (2006) also demonstrated the potential of fit evaluations using a static headform and breathing system, as the results from both small (0.096m3) and large (24.3m3) test chambers were essentially the same. However, further study is needed to validate robotic headform-based fit evaluation methods.
3.2.2 Simulation-based fit evaluation method
The fit of FFRs is evaluated in simulated virtual environments by investigating measures such as geometric similarity, overlapping areas, and contact pressure between digital face models and respirators. First, the geometric similarity can be used to predict the fit of a respirator by visually inspecting and calculating the space between the respirator's boundary and the face (Chu et al., 2015; Luximon et al., 2016). Second, the overlapping areas can be used to examine the fit of a respirator by virtually overlapping the respirator to the face and calculating the Euclidean distance between them (Lee et al., 2013; Visscher et al., 2015). Lastly, the contact pressure can be estimated by finite element analysis based on the mechanical properties of the deformable face models constructed for the respirator fit evaluation (Barros et al., 2014; Bader et al., 2019; Dai et al., 2011; Lei et al., 2012; Lee et al., 2020; Worsley et al., 2016; Yang et al., 2009).
Some studies have examined the validation of simulation results in mask design research using experimental methods, while the rest did not examine issues of validation while reporting their models and findings. Chu et al. (2015) validated a fully automatic design method developed for mass customization of a respiratory mask using a parametric face model by estimating the geometric similarity between the respirator and the wearer's face in a series of 10-fold cross-validation tests. Luximon et al. (2016) discussed the effectiveness of a design tool that provides 3D head templates in the Solidworks CAD environment by an overall satisfaction test with participants to a facemask designed using a median 3D head template. Visscher et al. (2015) conducted a prospective cohort study to examine the distance between the face and mask as a contributing factor to skin compromises such as excess skin hydration and pressure ulcer by measuring the distances between face scans at about 20 points on the surface of a mask such as nasal mask, oronasal mask, and total face mask. Lastly, Lei et al. (2014) validated an estimation algorithm of the contact area between respirator and headform by identifying a linear regression (R2 = 0.98) between simulation results and experimental measurements for headforms and respirators in various sizes. In contrast, Yang et al. (2009) and Dai et al. (2011) developed a simulation model using the finite element (FE) software LS-DYNA to examine the interaction between a respirator and a headform such as a strap tension, strap orientation, strap location, and seal material, but did not examine the verification or validation of the simulation results. Barros et al. (2014) used a 3D computational model to evaluate the main pressure zones of an oronasal interface on the face without verifying simulation results. Lastly, Lee et al. (2020) presented a computation model and a novel product design approach using template registration and FE analysis methods for proper contact pressure between the face and a wearable product without examining the validation of the proposed approach.
3.3 Comparison of human-based and Non-human based fit evaluation methods
The positive and negative features of the human-based and non-human based fit evaluation methods were compared in terms of convenience, cost-effectiveness, representativeness, and applicability (Table 2). First, human-based fit evaluations can provide a realistic simulation of respirator usage by incorporating human facial features and movements, but they cannot be used in hazardous environments and high concentrations (Bergman et al., 2014; Bergman et al., 2015). In contrast, non-human based methods can be used to conduct experiments with hazardous aerosols (e.g., silver nanoparticles, pathogenic microorganisms, and industrial aerosols) and high concentrations, but it is still a challenge for non-human based methods to simulate human facial features (e.g., skin softness, thickness, and hardness) and dynamic movements (e.g., speaking), although robotic headform and digital headform to simulate human facial features and dynamic movements were developed (Bergman et al., 2014; Bergman et al., 2015; He et al., 2014; Seo et al., 2020). Second, non-human based methods using simulation methods show more convenience because no human subjects and physical FFR prototypes are involved (Bergman et al., 2014; Wander, 2012; Yang et al., 2009).
Human-based methods, on the other hand, have various requirements such as approval from an institutional review board, refrain from smoking, and a rest period between experiments due to fatigue (Foereland et al., 2019; Yang et al., 2009). Last, experimental fit evaluation methods such as human-based and headform-based methods require a physical respirator prototype, which tends to be time-demanding and expensive. In addition, the current objective experimental methods only evaluate the overall fit, while the simulation-based method can locate unfit regions (Yang et al., 2009).
3.4 Statistical methods for validation analysis
Fit evaluation methods are validated by comparing them with reference human-based protocols using statistical analysis methods such as ROC, mean difference, correlation, and regression analysis. First, the effectiveness of a method in correctly identifying poorly fitting respirators is evaluated through ROC analysis with recommended values of test sensitivity ≥ 0.95, test specificity > 0.50, the predictive value of pass ≥ 0.95, and predictive value of fail > 0.50. In addition, the degree of agreement can be evaluated by Kappa (K) value, with a recommended value of K value > 0.70 (ANSI/AIHA Z88.10, 2010; Coffey et al., 2002; Grinshpun et al., 2021; Rengasamy et al., 2014; Sietsema and Brosseau, 2018; Sreenath et al., 2001). Second, mean difference analysis can be used to compare the results of two fit evaluation protocols (Sietsema and Brosseau, 2016). For example, Sietsema and Brosseau (2016) evaluated the FF of two protocols for each exercise and all exercises combined and no significant difference was found. In addition, correlation analysis can also be conducted to compare two protocols (Bergman et al., 2015; Kim et al., 2016; Sietsema and Brosseau, 2018). For example, Sietsema and Brosseau (2018) evaluated a fit testing scenario during realistic healthcare activities using an SWPF by analyzing the correlations of SWPFs and FFs (Sietsema and Brosseau, 2018). Finally, regression analysis can be employed for evaluating a fit evaluation method (ANSI/AIHA Z88.10, 2010; Nelson and Mullins, 2004). For example, a binary logistic regression analysis can be used to assess the probability of passing a fit evaluation as a function of a reference FF (ANSI/AIHA Z88.10, 2010).
The present study conducted a comprehensive review of fit evaluation methods for FFRs. The fit evaluation methods were summarized into human-based and non-human-based (headform and simulation) evaluations. Human-based methods have been widely adopted and implemented in subjective and objective ways as national standards, while non-human-based methods are still in their developmental stage and require further validation. A comparison of the positive and negative features of the two methods was conducted in terms of convenience, cost-effectiveness, representativeness, and applicability.
The development of non-human based fit evaluation methods for FFRs should be a priority due to their advantages in terms of convenience, representativeness, and applicability compared to human-based evaluation methods (Bergman et al., 2014; Brosseau et al., 2010; Foereland et al., 2019; Wander, 2012; Yang et al., 2009). First, non-human based methods are more convenient as they require fewer physical human resources, reducing the complexities of requirements such as approval from an institutional review board, scheduling of experiments, recruitment of participants, and administration of experiments (Bergman et al., 2014; Brosseau et al., 2010; Foereland et al., 2019; Wander, 2012; Yang et al., 2009). Additionally, non-human based methods offer advanced simulations of real-world conditions, resulting in a more representative evaluation. For example, headform-based experiments can be used to simulate real-world conditions that are difficult to replicate on human subjects due to ethical and safety concerns, such as testing for pediatric populations, long-term duration, very high aerosol concentrations, and hazardous aerosols (Bergman et al., 2015; Hauge et al., 2012). Lastly, simulation-based methods can objectively identify the unfit area of the contact area between the face and FFRs, enabling improvements in respirator design and use (Yang et al., 2019).
The development of non-human based fit evaluation methods requires further improvement, although they have gained attention over human-based methods because of their various advantages. Recent studies have developed and preliminarily validated several new non-human based methods as alternatives to human-based methods (Bergman et al., 2014; Lei et al., 2014). It is necessary to ensure that non-human based fit methods can adequately represent realistic human factors (e.g., facial features and breath modes), real-world respirator wearing conditions (e.g., dynamic movements and hazardous environments), and provide accurate feedback on unfit conditions (e.g., specific unfit areas and local unfit levels). First, anthropometric features of a specific population should be considered for the development of headforms and digital head models. Next, simulation-based methods commonly lack the exercise protocols, which should be developed and validated with real-world human activities. Lastly, the headform-based and the simulation-based methods require the development of an unfit facial feedback function, which would enable the identification of the unfit areas and levels between the headform and FFRs.
This study offers comprehensive information on FFR fit evaluation methods, which can serve as a guide for the development and utilization of fit evaluation methods. It highlights the need for developing more non-human-based fit evaluation methods as an alternative to the predominantly used human-based methods for various contexts. It is worth noting that the study specifically concentrates on fit evaluation methods for FFRs and does not encompass other types of masks, such as elastomeric facepiece respirators. However, the findings presented in this study can serve as a valuable reference for future research on fit evaluation methods for other mask types, providing useful insights and recommendations.
References
1. ANSI, ANSI/AIHA Z88.10 American National Standards Institute: American National Standard for Respiratory Protection, American National Standards Institute, New York, 2010.
2. Bader, D.L., Worsley, P.R. and Gefen, A., Bioengineering considerations in the prevention of medical device-related pressure ulcers, Clinical Biomechanics, 67, 70-77, 2019. doi: 10.1016/j.clinbiomech.2019.04.018.
Google Scholar
3. Bałazy, A., Toivola, M., Reponen, T., Podgórski, A., Zimmer, A. and Grinshpun, S.A., Manikin-based performance evaluation of N95 filtering-facepiece respirators challenged with nanoparticles, Annals of Occupational Hygiene, 50(3), 259-269, 2006. doi: 10.1093/ annhyg/mei058.
Google Scholar
4. Barros, L.S., Talaia, P., Drummond, M. and Natal-Jorge, R., Facial pressure zones of an oronasal interface for noninvasive ventilation: a computer model analysis, Jornal Brasileiro de Pneumologia, 40, 652-657, 2014. doi: 10.1590/S1806-37132014000600009.
5. Bergman, M.S., Viscusi, D.J., Zhuang, Z., Palmiero, A.J., Powell, J.B. and Shaffer, R.E., Impact of multiple consecutive donnings on filtering facepiece respirator fit, American Journal of Infection Control, 40(4), 375-380, 2012. doi: 10.1016/j.ajic.2011.05.003.
Google Scholar
6. Bergman, M.S., Zhuang, Z., Hanson, D., Heimbuch, B.K., McDonald, M.J., Palmiero, A.J., Shaffer, R.E., Harnish, D., Husband, M. and Wander, J.D., Development of an advanced respirator fit-test headform, Journal of Occupational and Environmental Hygiene, 11(2), 117-125, 2014. doi: 10.1080/15459624.2013.816434.
Google Scholar
7. Bergman, M.S., He, X., Joseph, M.E., Zhuang, Z., Heimbuch, B.K., Shaffer, R.E., Choe, M. and Wander, J.D., Correlation of respirator fit measured on human subjects and a static advanced headform, Journal of Occupational and Environmental Hygiene, 12(3), 163-171, 2015. doi: 10.1080/15459624.2014.957832.
Google Scholar
8. Bergman, M., Basu, R., Lei, Z., Niezgoda, G. and Zhuang, Z., Development of a manikin-based performance evaluation method for loose-fitting powered air-purifying respirators, Journal of the International Society for Respiratory Protection, 34(1), 40, 2017.
Google Scholar
9. Brosseau, L.M., Fit testing respirators for public health medical emergencies, Journal of Occupational and Environmental Hygiene, 7(11), 628-632, 2010. doi: 10.1080/15459624.2010.514782.
Google Scholar
10. Canadian Standards Association (CSA), Selection, Use, and Care of Respirators, CSA-Z94.4-18, 2018, https://www.csagroup.org/ store/product/CAN-CSA-Z94.4-18/.
11. Chu, C.H., Huang, S.H., Yang, C.K. and Tseng, C.Y., Design customization of respiratory mask based on 3D face anthropometric data, International Journal of Precision Engineering and Manufacturing, 16, 487-494, 2015. doi: 10.1007/s12541-015-0066-5.
Google Scholar
12. Ciotti, C., Pellissier, G., Rabaud, C., Lucet, J.C., Abiteboul, D. and Bouvet, E., Effectiveness of respirator masks for healthcare workers, in France, Medecine et Maladies Infectieuses, 42(6), 264-269, 2012. doi: 10.1016/j.medmal.2012.05.001.
Google Scholar
13. Clapp, P.W., Sickbert-Bennett, E.E., Samet, J.M., Berntsen, J., Zeman, K.L., Anderson, D.J., Weber, D.J. and Bennett, W.D., Evaluation of cloth masks and modified procedure masks as personal protective equipment for the public during the COVID-19 pandemic, JAMA Internal Medicine, 181(4), 463-469, 2021. doi: 10.1001/jamainternmed.2020.8168.
Google Scholar
14. Clayton, M. and Vaughan, N., Fit for purpose? The role of fit testing in respiratory protection, Annals of Occupational Hygiene, 49(7), 545-548, 2005. doi: 10.1093/annhyg/mei046.
Google Scholar
15. Coffey, C.C., Zhuang, Z., Campbell, D.L. and Myers, W.R., Quantitative fit-testing of N95 respirators: Part II-Results, effect of filter penetration, fit-test, and pass/fail criteria on respirator performance, Journal of International Society for Respiratory Protection, 16(1/4), 25-36, 1998.
16. Coffey, C.C., Lawrence, R.B., Zhuang, Z., Campbell, D.L., Jensen, P.A. and Myers, W.R., Comparison of five methods for fit-testing N95 filtering-facepiece respirators, Applied Occupational and Environmental Hygiene, 17(10), 723-730, 2012. doi: 10.1080/ 10473220290107002.
Google Scholar
17. Colton, C.E., Respirator fit testing: choosing the best method, Metal Finishing, 99(9), 53-55, 2001. doi: 10.1016/S0026-0576(01)81436-7.
Google Scholar
18. Cui, X., Jung, H., Lee, W., Kim, S.H., Yun, R.Y., Kim, S.Y., You, H. and Huh, S., Ergonomics and personalization of noninvasive ventilation masks, Respiratory Care, 67(1), 87-101, 2022. doi: 10.4187/respcare.08959.
Google Scholar
19. Dai, J., Yang, J.J. and Zhuang, Z., Sensitivity analysis of important parameters affecting contact pressure between a respirator and a headform, International Journal of Industrial Ergonomics, 41(3), 268-279, 2011. doi: 10.1016/j.ergon.2011.01.007.
Google Scholar
20. Davidson, C.S., Green, C.F., Gibbs, S.G., Schmid, K.K., Panlilio, A.L., Jensen, P.A. and Scarpino, P.V., Performance evaluation of selected N95 respirators and surgical masks when challenged with aerosolized endospores and inert particles, Journal of Occupational and Environmental Hygiene, 10(9), 461-467, 2013. doi: 10.1080/15459624.2013.818243.
Google Scholar
21. Elmashae, R.B.Y., Grinshpun, S.A., Reponen, T., Yermakov, M. and Riddle, R., Performance of two respiratory protective devices used by home-attending health care workers (a pilot study), Journal of Occupational and Environmental Hygiene, 14(9), D145-D149, 2017. doi: 10.1080/15459624.2017.1319571.
Google Scholar
22. Fakherpour, A., Jahangiri, M., Yousefinejad, S. and Seif, M., Feasibility of replacing homemade solutions by commercial products for qualitative fit testing of particulate respirators: A mixed effect logistic regression study, MethodsX, 6, 1313-1322, 2019. doi: 10.1016/j.mex.2019.05.034.
Google Scholar
23. Fakherpour, A., Jahangiri, M., Seif, M., Charkhand, H., Abbaspour, S. and Floyd, E.L., Quantitative fit testing of filtering face-piece respirators during the COVID-19 pandemic reveals anthropometric deficits in most respirators available in Iran, Journal of Environmental Health Science and Engineering, 19, 805-817, 2021. doi: 10.1007/s40201-021-00648-3.
Google Scholar
24. Foereland, S., Robertsen, O. and Hegseth, M.N., Do various respirator models fit the workers in the Norwegian Smelting Industry?, Safety and Health at Work, 10(3), 370-376, 2019. doi: 10.1016/j.shaw.2019.06.004.
Google Scholar
25. Government of Western Australia (WA Government), Department of Health and Public and Aboriginal Heath Division, Respiratory Protection Guidelines for Western Australian Healthcare Facilities, 2022, https://ww2.health.wa.gov.au/~/media/Corp/Documents/ Health-for/Infectious-disease/HISWA/RPPWAHCFCDCDGuideline V10July2022.pdf.
26. Grinshpun, S.A., Haruta, H., Eninger, R.M., Reponen, T., McKay, R.T. and Lee, S.A., Performance of an N95 filtering facepiece particulate respirator and a surgical mask during human breathing: two pathways for particle penetration, Journal of Occupational and Environmental Hygiene, 6(10), 593-603, 2009. doi: 10.1080/15459620903120086.
Google Scholar
27. Grinshpun, S.A., Yermakov, M. and Kano, M., Evaluation of AccuFIT 9000: a novel apparatus for quantitative fit testing of particulate respirators, Annals of Work Exposures and Health, 65(4), 458-462, 2021. doi: 10.1093/annweh/wxaa116.
Google Scholar
28. Han, D.H., Inward leakage test for particulate filtering respirators in Korea, Journal of Environmental Health Sciences, 30(5), 432-439, 2004.
Google Scholar
29. Han, D.H. and Lee, J., Evaluation of particulate filtering respirators using inward leakage (IL) or total inward leakage (TIL) testing—Korean experience, Annals of Occupational Hygiene, 49(7), 569-574, 2005. doi: 10.1093/annhyg/mei034.
Google Scholar
30. Han, D.H., Usage of filtering-facepiece masks for healthcare workers and importance of fit testing, Journal of Korean Society of Occupational and Environmental Hygiene, 25(3), 245-253, 2015. doi: 10.15269/JKSOEH.2015.25.3.245.
31. Hauge, J., Roe, M., Brosseau, L.M. and Colton, C., Real-time fit of a respirator during simulated health care tasks, Journal of Occupational and Environmental Hygiene, 9(10), 563-571, 2012. doi: 10.1080/15459624.2012.711699.
Google Scholar
32. He, X., Yermakov, M., Reponen, T., McKay, R.T., James, K. and Grinshpun, S.A., Manikin-based performance evaluation of elastomeric respirators against combustion particles, Journal of Occupational and Environmental Hygiene, 10(4), 203-212, 2013. doi: 10.1080/ 15459624.2012.760063.
Google Scholar
33. He, X., Grinshpun, S.A., Reponen, T., McKay, R., Bergman, M.S. and Zhuang, Z., Effects of breathing frequency and flow rate on the total inward leakage of an elastomeric half-mask donned on an advanced manikin headform, Annals of Occupational Hygiene, 58(2), 182-194, 2014. doi: 10.1093/annhyg/met053.
Google Scholar
34. ISO, Respiratory Protective Devices-Selection, Use and Maintenance: Part 3—Fit Testing Procedures, ISO 16975-3, 2017.
35. ISO, Respiratory Protective Devices - Methods of Test and Test Equipment—Part 1: Determination of Inward Leakage, ISO 16900-1, 2019.
36. Jung, J.Y. and Lee, J.Y., Comparison of fit factor and total inward leakage of face masks: exploratory evaluation by mask designs and face panels, Journal of Korean Living Environment System, 28(4), 377-390, 2021. doi: 10.21086/ksles.2021.8.28.4.377.
Google Scholar
37. Karuppasamy, K. and Obuchowski, N., Comparison of fit for sealed and loose-fitting surgical masks and N95 filtering facepiece respirators, Annals of Work Exposures and Health, 65(4), 463-474, 2021. doi: 10.1093/annweh/wxaa125.
Google Scholar
38. KFDA, Guideline on Standards and Specifications for Filtering Respirators (for industry), 2019. https://www.mfds.go.kr/eng/brd/ m_65/down.do?brd_id=engcovid1902&seq=6&data_tp=A&file_seq=1.
39. Kim, H., Baek, J.E., Seo, H.K., Lee, J.E., Myong, J.P., Lee, S.J. and Lee, J.H., Assessing real-time performances of N95 respirators for health care workers by simulated workplace protection factors, Industrial Health, 53(6), 553-561, 2015. doi: 10.2486/ndhealth.2014-0259.
Google Scholar
40. Kim, J.H., Wu, T., Powell, J.B. and Roberge, R.J., Physiologic and fit factor profiles of N95 and P100 filtering facepiece respirators for use in hot, humid environments, American Journal of Infection Control, 44(2), 194-198, 2016. doi: 10.1016/j.ajic.2015.08.027.
Google Scholar
PubMed
41. Kim, J.K., Filtration efficiency and manikin-based total inward leakage study of particle filtering mask challenged with silver nanoparticles, Journal of Korean Society of Occupational and Environmental Hygiene, 26(3), 367-376, 2016. doi: http://dx.doi.org/ 10.15269/JKSOEH.2016.26.3.367.
42. Lawrence, R.B., Duling, M.G., Calvert, C.A. and Coffey, C.C., Comparison of performance of three different types of respiratory protection devices, Journal of Occupational and Environmental Hygiene, 3(9), 465-474, 2006. doi: 10.1080/15459620600829211.
Google Scholar
43. Lee, W., Kim, H., Jung, D., Park, S. and You, H., "Ergonomic design and evaluation of a pilot oxygen mask", In Proceedings of the Human Factors and Ergonomics Society Annual Meeting, 57(1) (pp. 1673-1677), Los Angeles, CA, 2013.
Google Scholar
44. Lee, W., Kim, J.G., Molenbroek, J.M., Goossens, R.H. and You, H., Estimation of facial contact pressure based on finite element analysis, In Proceedings of the AHFE 2019 International Conference on Additive Manufacturing, Modeling Systems and 3D Prototyping, 10 (pp. 657-667), Washington DC, USA, 2020.
Google Scholar
45. Lei, Z., Yang, J. and Zhuang, Z., Headform and N95 filtering facepiece respirator interaction: contact pressure simulation and validation. Journal of Occupational and Environmental Hygiene, 9(1), pp. 46-58, 2012. doi: 10.1080/15459624.2011.635130.
Google Scholar
46. Lei, Z., Ji, X., Li, N., Yang, J., Zhuang, Z. and Rottach, D., Simulated effects of head movement on contact pressures between headforms and N95 filtering facepiece respirators-part 1: headform model and validation, Annals of Occupational Hygiene, 58(9), 1175-1185, 2014.
Google Scholar
47. Luximon, Y., Ball, R.M. and Chow, E.H., A design and evaluation tool using 3D head templates, Computer-Aided Design and Applications, 13(2), 153-161, 2016. doi: 10.1080/16864360.2015.1084188.
Google Scholar
48. Manganyi, J., Wilson, K.S. and Rees, D., Quantitative respirator fit, face sizes, and determinants of fit in South African diagnostic laboratory respirator users, Annals of Work Exposures and Health, 61(9), 1154-1162, 2017. doi: 10.1093/annweh/wxx077.
Google Scholar
49. Nelson, J. and Mullins, E., Recommendations for the acceptance criteria for new fit test methods, Journal of the International Society for Respiratory Protection, 21, 1-10, 2004.
50. NIOSH, Total Inward Leakage Test for Half-Mask Air-Purifying Particulate Respirator, NIOSH RCT-APR-STP-0068, http://www.cdc.gov/ niosh/docket/archive/pdfs/NIOSH-137/0137-081209-DraftTIL.pdf.
51. OHS, OHS Guidelines Part 8: Personal Protective Clothing and Equipment, 2020. https://www.worksafebc.com/en/law-policy/ occupational-health-safety/searchable-ohs-regulation/ohs-guidelines/guidelines-part-08.
52. Or, P., Chung, J. and Wong, T., A novel approach to fit testing the N 95 respirator in real time in a clinical setting, International Journal of Nursing Practice, 22(1), 22-30, 2016. doi: 10.1111/ijn.12354.
Google Scholar
53. OSHA, Respiratory Protection Program Standards-Fit Testing Procedures (Mandatory), Title 29 CFR.1910.134, 2021. https:// www.osha.gov/laws-regs/regulations/standardnumber/1910/1910.134AppA.
54. Pacitto, A., Amato, F., Salmatonidis, A., Moreno, T., Alastuey, A., Reche, C., Buonanno, G., Benito, C. and Querol, X., Effectiveness of commercial face masks to reduce personal PM exposure, Science of the Total Environment, 650, 1582-1590, 2019. doi: 10.1016/ j.scitotenv.2018.09.109.
55. Pan, X., Li, X., Kong, P., Wang, L., Deng, R., Wen, B., Xiao, L., Song, H., Sun, Y., Zhou, H., Lu, J., Wang, Y., Gui, Q., Duo, L. and Sun, C., Assessment of use and fit of face masks among individuals in public during the COVID-19 pandemic in China, JAMA Network Open, 4(3), e212574-e212574, 2021. doi: 10.1001/jamanetworkopen.2021.2574.
Google Scholar
56. Park, J.J., Seo, Y.B. and Lee, J., Fit test for N95 filtering facepiece respirators and KF94 masks for healthcare workers: a prospective single-center simulation study, Journal of Korean Medical Science, 36(21), 2021. doi: 10.3346/jkms.2021.36.e140.
Google Scholar
57. Regli, A., Sommerfield, A. and von Ungern-Sternberg, B.S., The role of fit testing N95/FFP2/FFP3 masks: a narrative review, Anaesthesia, 76(1), 91-100, 2021. doi: 10.1111/anae.15261.
Google Scholar
58. Rengasamy, S., Walbert, G.F., Newcomb, W.E., Faulkner, K., Rengasamy, M.M., Brannen, J.J. and Szalajda, J.V., Total inward leakage measurement of particulates for N95 filtering facepiece respirators—a comparison study, Annals of Occupational Hygiene, 58(2), 206-216, 2014. doi: 10.1093/annhyg/met054.
Google Scholar
59. Rengasamy, S., Zhuang, Z., Niezgoda, G., Walbert, G., Lawrence, R., Boutin, B., Hudnall, J., Monaghan, W.P., Miller, C., Harris, J. and Coffey, C., A comparison of total inward leakage measured using sodium chloride (NaCl) and corn oil aerosol methods for air-purifying respirators, Journal of Occupational and Environmental Hygiene, 15(8), 616-627, 2018. doi: 10.1080/15459624.2018.1479064.
Google Scholar
60. Reponen, T., Lee, S.A., Grinshpun, S.A., Johnson, E. and Mckay, R., Effect of fit testing on the protection offered by N95 filtering facepiece respirators against fine particles in a laboratory setting, Annals of Occupational Hygiene, 55(3), 264-271, 2011. doi: 10.1093/annhyg/meq085.
Google Scholar
61. Robertson, S. and Ramsdale, M.P., Audit of qualitative fit testing for FFP3 respirators, British Dental Journal, 1-4, 2021. doi: 10.1038/s41415-021-2716-6.
Google Scholar
62. Rollings, L., FFP3 respirator face fit testing-what is it all about?, Bdj Team, 7(8), 30-33, 2020, doi: 10.1038/s41415-020-1850-x.
Google Scholar
63. Seo, H., Kim, J.I. and Kim, H., Development of Korean head forms for respirator performance testing, Safety and Health at Work, 11(1), 71-79, 2020. doi: 10.1016/j.shaw.2019.12.008.
Google Scholar
64. Sietsema, M. and Brosseau, L.M., Comparison of two quantitative fit-test methods using N95 filtering facepiece respirators. Journal of Occupational and Environmental Hygiene, 13(8), 621-627, 2016. doi: 10.1080/15459624.2016.1159690.
Google Scholar
65. Sietsema, M. and Brosseau, L.M., Are quantitative fit factors predictive of respirator fit during simulated healthcare activities?, Journal of Occupational and Environmental Hygiene, 15(12), 803-809, 2018. doi: 10.1080/15459624.2018.1515490.
Google Scholar
66. Spies, A., Wilson, K.S. and Ferrie, R., Respirator fit of a medium mask on a group of South Africans: a cross-sectional study, Environmental Health, 10, 1-7, 2011. doi: 10.1186/1476-069X-10-17.
Google Scholar
67. Sreenath, A., Weed, J. and Church, T., A modified protocol for quantitative fit testing using the PortaCount®, Applied Occupational and Environmental Hygiene, 16(10), 979-988, 2001. doi: 10.1080/104732201300367245.
68. Sun, C., Thelen, C., Sanz, I.S. and Wittmann, A., Real-time performance of filtering facepiece respirators at the workplace, Gefahrstoffe Reinhaltung Der Luft, 79(10), 378-384, 2019. doi: 10.37544/0949-8036-2019-10-20.
69. Visscher, M.O., White, C.C., Jones, J.M., Cahill, T., Jones, D.C. and Pan, B.S., Face masks for noninvasive ventilation: fit, excess skin hydration, and pressure ulcers, Respiratory Care, 60(11), 1536-1547, 2015. doi: 10.4187/respcare.04036.
Google Scholar
70. Wander, J., Hanson, D. and Margolin, R., Humanlike articulate robotic headform to replace human volunteers in respirator fit testing, Han Robotics Inc Plano TX, 2012.
Google Scholar
71. Wardhan, R., Brennan, M.M., Brown, H.L. and Creech, T.B., Does a modified adhesive respirator improve the face seal for health care workers who previously failed a fit test?: A Pilot study during the coronavirus disease 2019 pandemic, A&A Practice, 14(8), e01264, 2020. doi: 10.1213/XAA.0000000000001264.
Google Scholar
PubMed
72. Worsley, P.R., Prudden, G., Gower, G. and Bader, D.L., Investigating the effects of strap tension during non-invasive ventilation mask application: a combined biomechanical and biomarker approach, Medical Devices: Evidence and Research, 409-417, 2016. doi: 10.2147/MDER.S121712.
Google Scholar
73. Yang, J., Dai, J. and Zhuang, Z., Simulating the interaction between a respirator and a headform using LS-DYNA, Computer-Aided Design and Applications, 6(4), 539-551, 2009. doi: 10.3722/cadaps.2009.539-551.
Google Scholar
74. Yao, B.G., Wang, Y.X., Ye, X.Y., Zhang, F. and Peng, Y.L., Impact of structural features on dynamic breathing resistance of healthcare face mask, Science of The Total Environment, 689, 743-753, 2019. doi: 10.1016/j.scitotenv.2019.06.463.
Google Scholar
75. Zhang, X., Lee, S.W. and Braido, P., Determining finger segmental centers of rotation in flexion-extension based on surface marker measurement, Journal of Biomechanics, 36(8), 1097-1102, 2003. doi: 10.1016/s0021-9290(03)00112-x.
Google Scholar
76. Zhuang, Z., Benson, S., Lynch, S., Palmiero, A. and Roberge, R., Laboratory study to assess causative factors affecting temporal changes in filtering Facepiece respirator fit: Part I–pilot study, Journal of Occupational and Environmental Hygiene, 8(12), 729-739, 2011. doi: 10.1080/15459624.2011.627294.
Google Scholar
77. Zhuang, Z., Liu, Y., Coffey, C.C., Miller, C. and Szalajda, J., Inward leakage variability between respirator fit test panels–Part I. Deterministic approach, Journal of Occupational and Environmental Hygiene, 12(11), 753-760, 2015. doi: 10.1080/ 15459624.2015.1047025.
Google Scholar
78. Zhuang, Z., Bergman, M., Brochu, E., Palmiero, A., Niezgoda, G., He, X., Roberge, R. and Shaffer, R., Temporal changes in filtering-facepiece respirator fit, Journal of Occupational and Environmental Hygiene, 13(4), 265-274, 2016. doi: 10.1080/ 15459624.2015.1116692.
Google Scholar
79. Zhuang, Z., Bergman, M., Lei, Z., Niezgoda, G. and Shaffer, R., Recommended test methods and pass/fail criteria for a respirator fit capability test of half-mask air-purifying respirators, Journal of Occupational and Environmental Hygiene, 14(6), 473-48, 2017. doi: 10.1080/15459624.2017.1296233.
Google Scholar
PIDS App ServiceClick here!